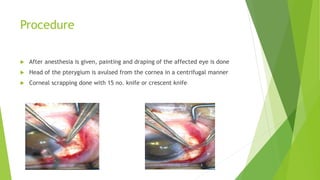
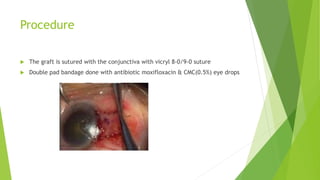
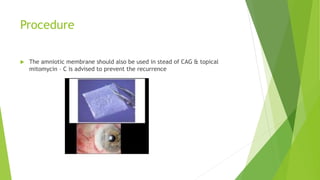
Pterygium is a triangular growth of conjunctival tissue that extends onto the cornea. It is caused by prolonged sun exposure and is more common in older males working outdoors. Symptoms include irritation, foreign body sensation, and decreased vision. Treatment options include conservative measures like artificial tears or surgical excision with conjunctival autograft to prevent recurrence. Surgery involves removing the pterygium tissue from the cornea and replacing it with a conjunctival graft taken from the patient's eye. Post-operative care and monitoring for recurrence is important.