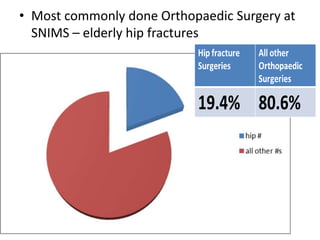
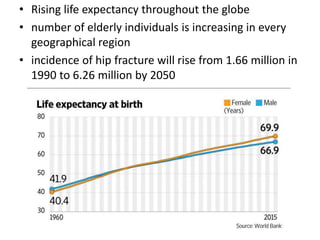
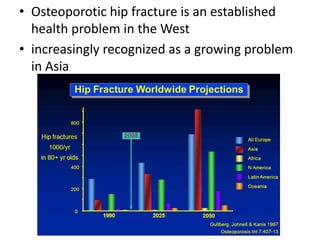
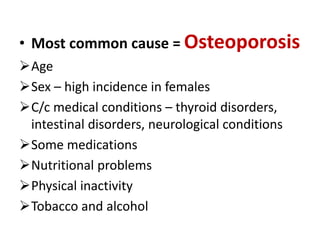
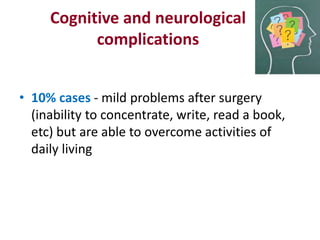
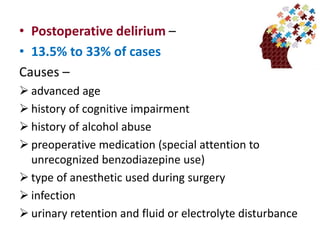
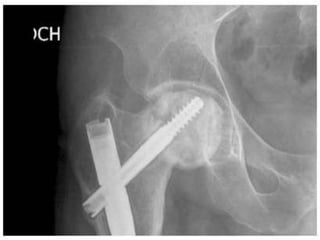
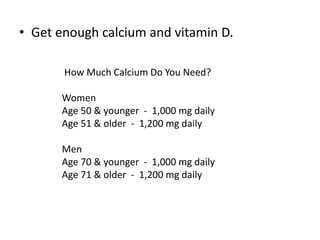
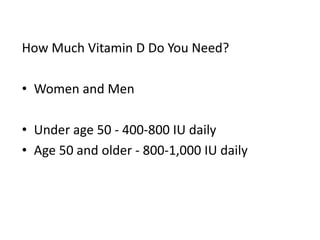
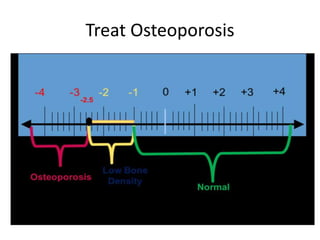
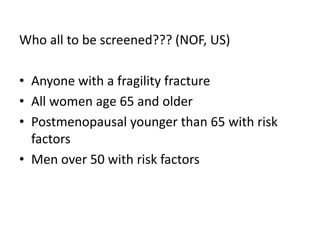
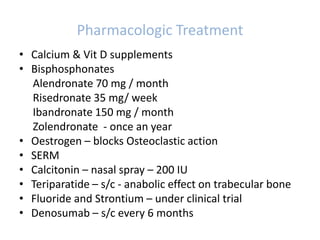
The document addresses the rising incidence of hip fractures in the elderly, primarily caused by osteoporosis, and outlines the associated complications, which include chronic pain, disability, and increased mortality. It emphasizes the importance of early surgical intervention within 48 hours to improve outcomes and discusses preventative measures such as healthy lifestyle choices, exercise, and osteoporosis screening. The document highlights the significant public health challenge posed by osteoporotic fractures, particularly as global life expectancy increases.