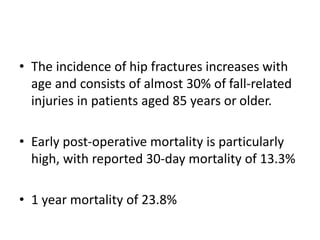
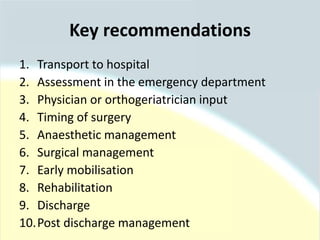
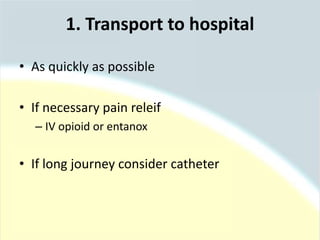
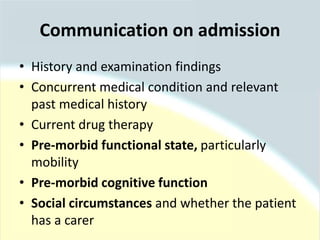
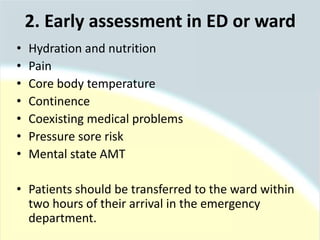
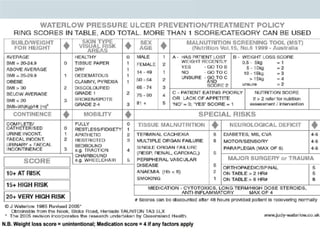
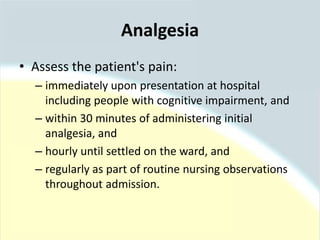
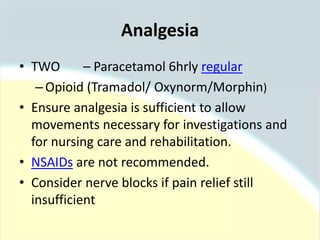
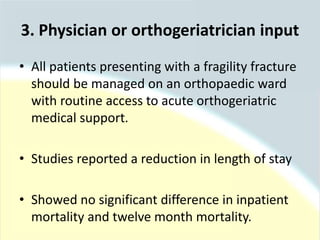
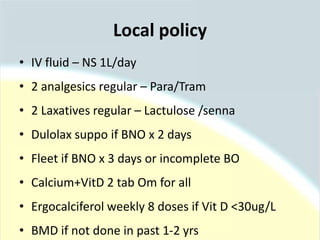
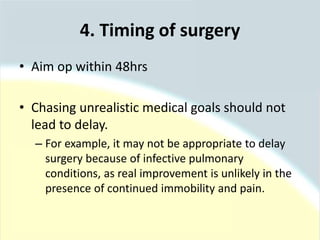
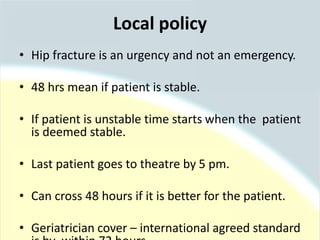
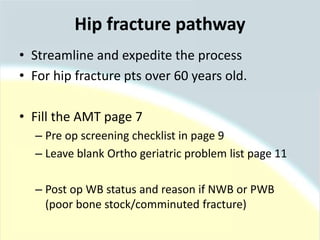
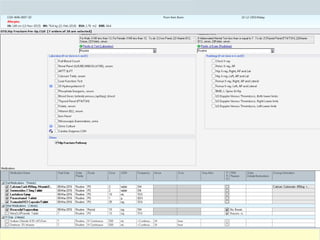
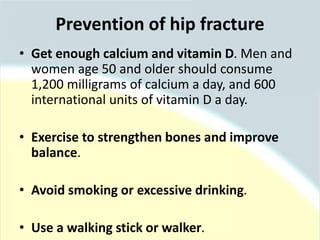
The document discusses guidelines for the management of hip fractures. It covers topics such as transport to the hospital, assessment in the emergency department, timing of surgery within 48 hours, rehabilitation starting within 24 hours of surgery, and post-discharge management including continued physical therapy. The management of hip fractures is a multidisciplinary process involving services across the healthcare system.