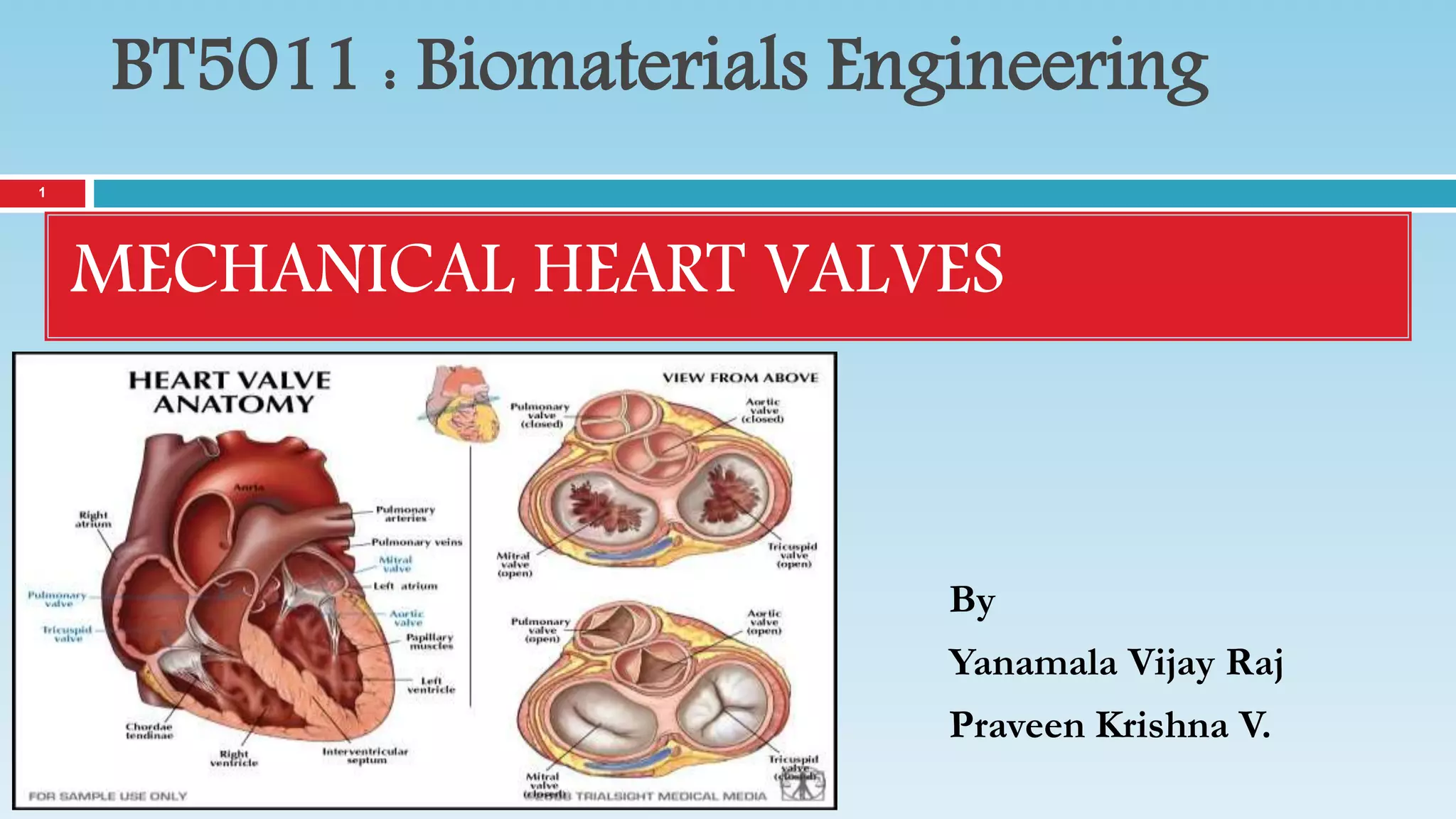
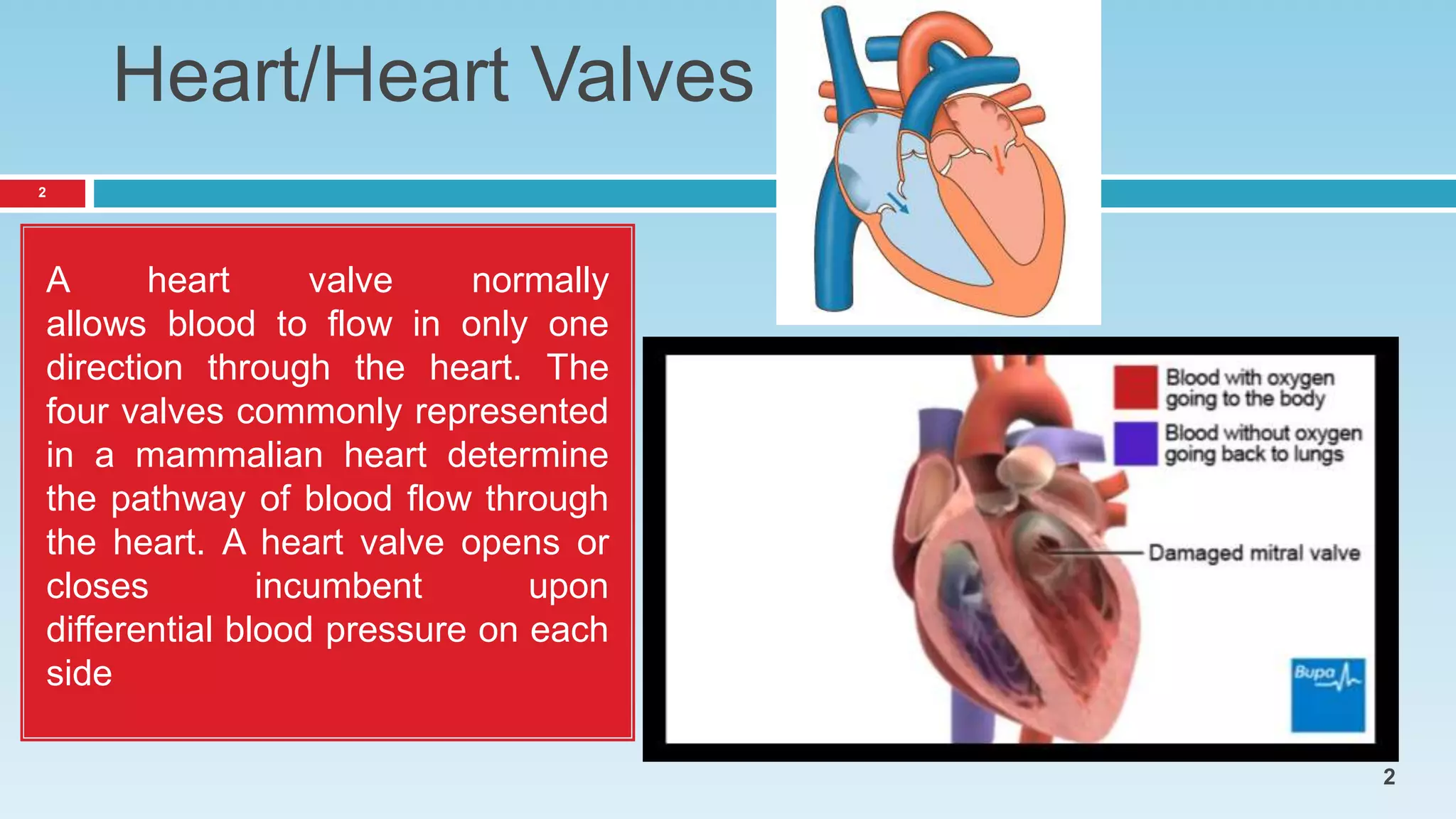
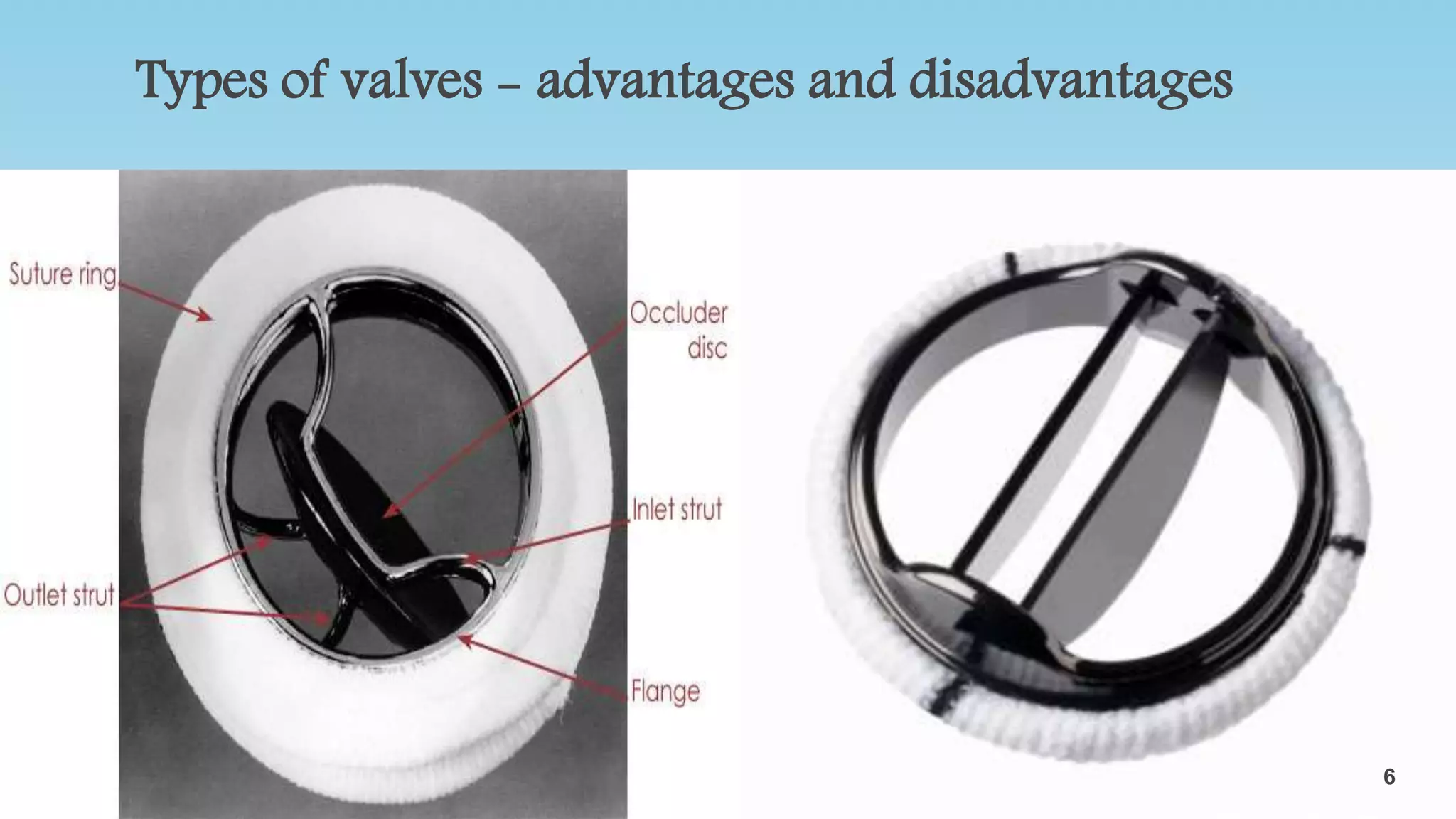
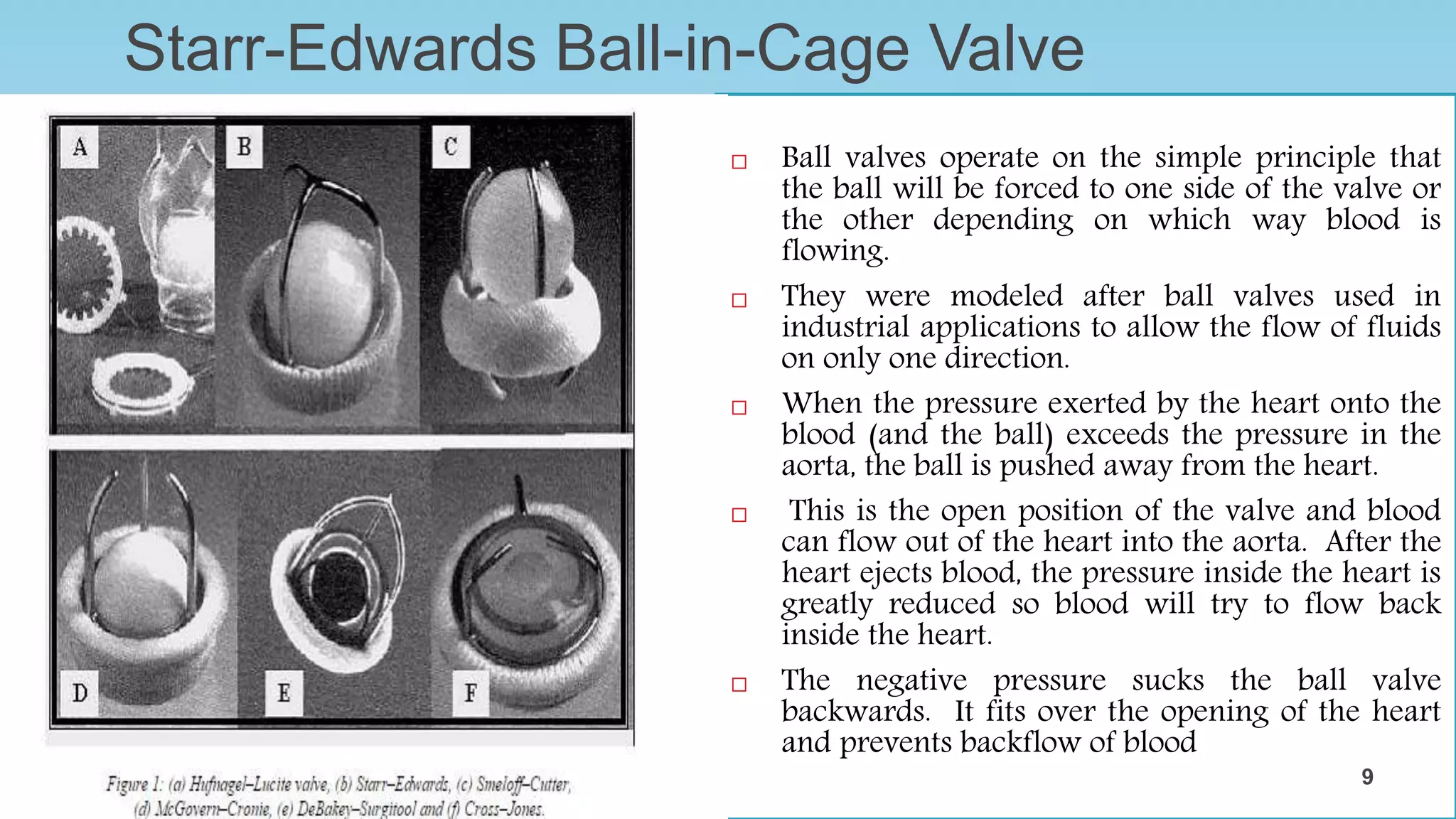
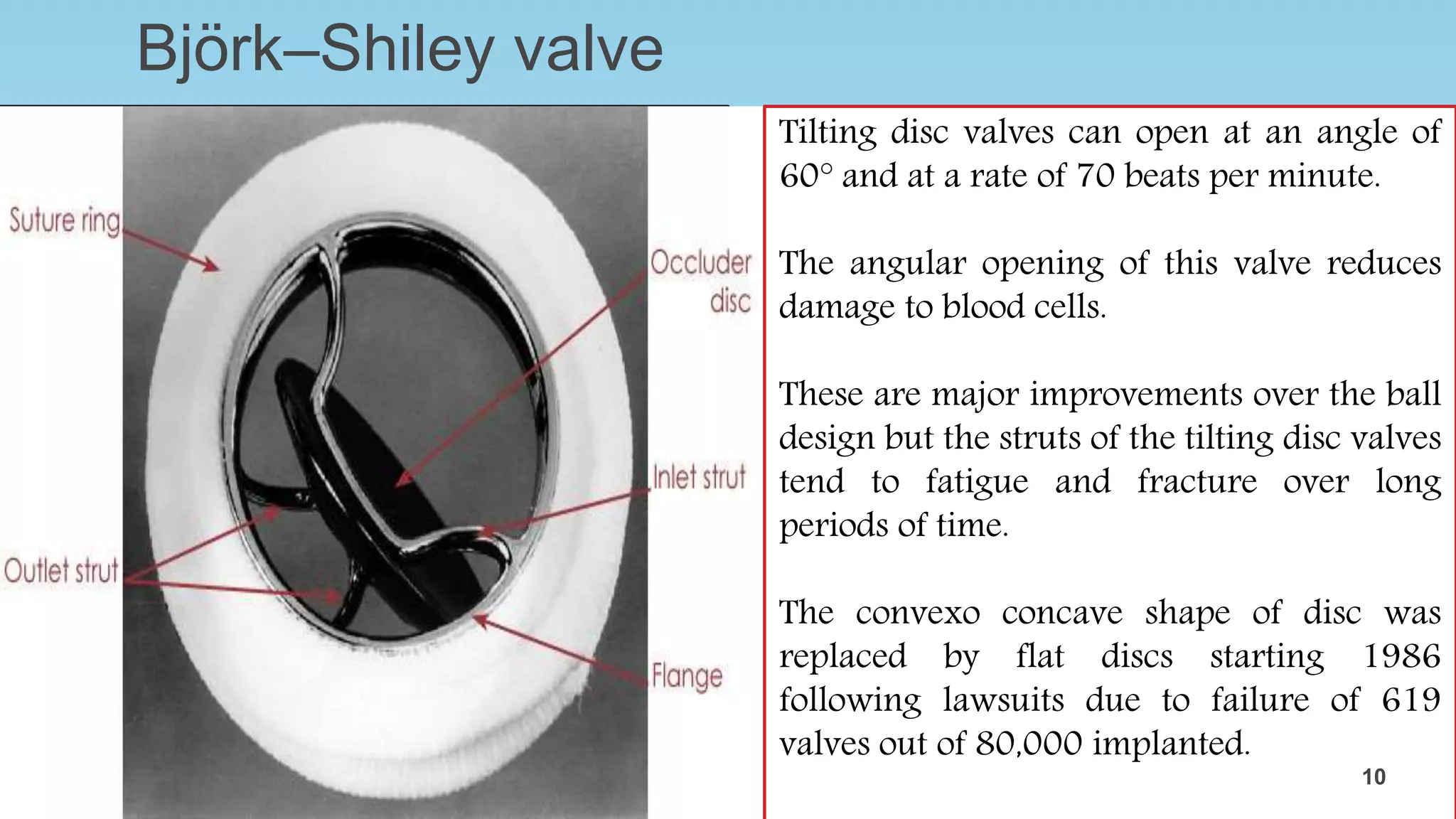
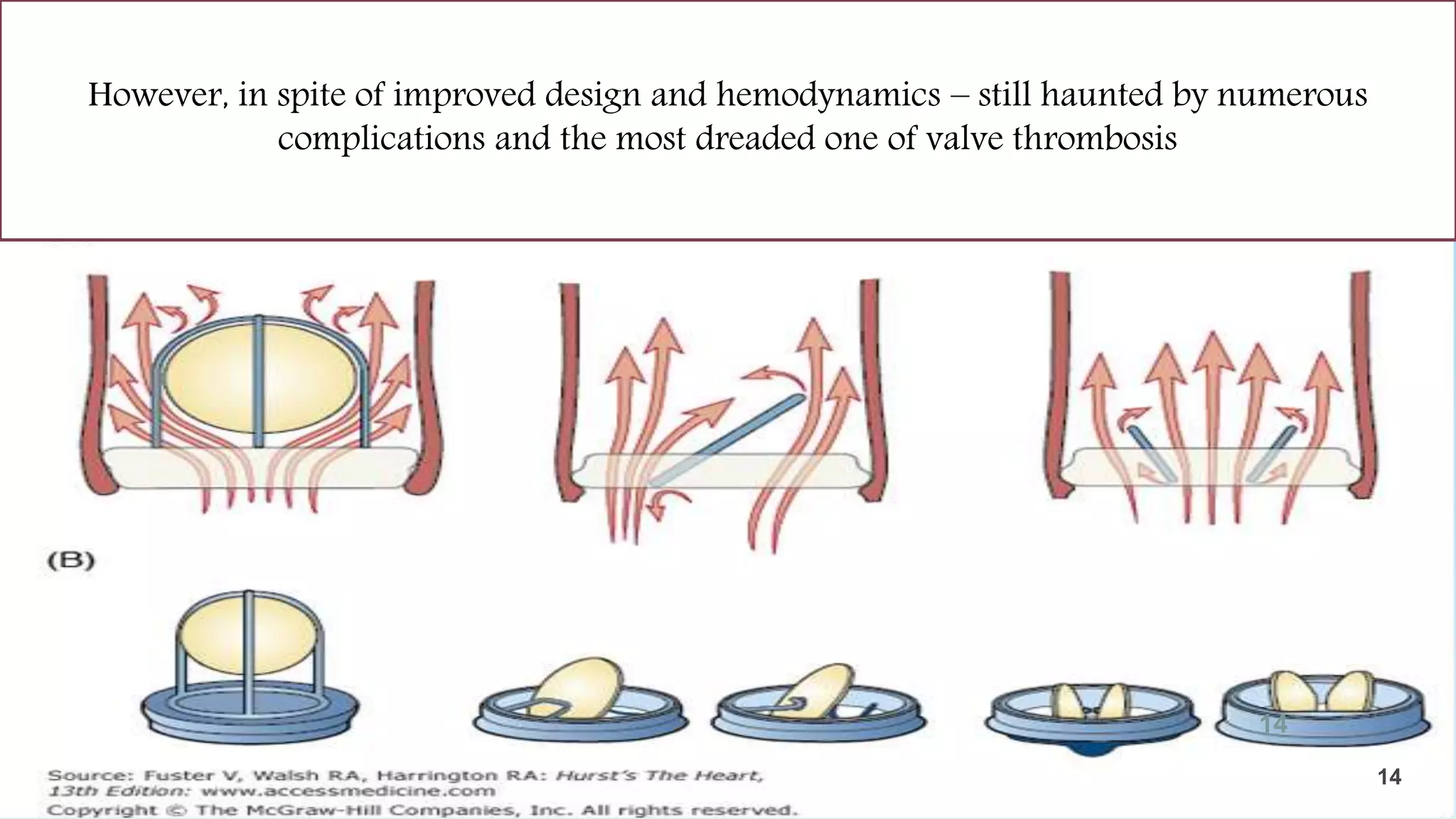
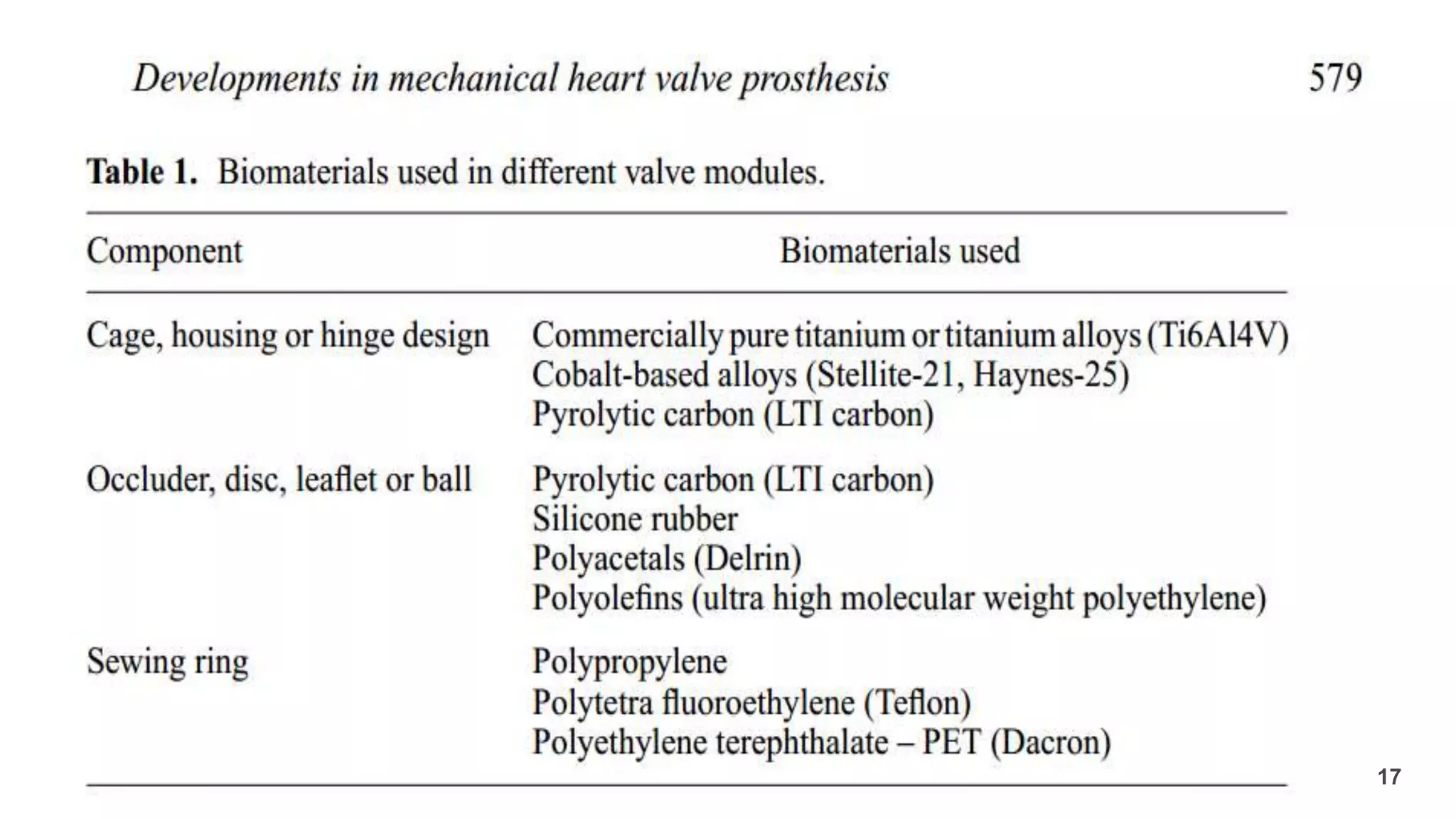
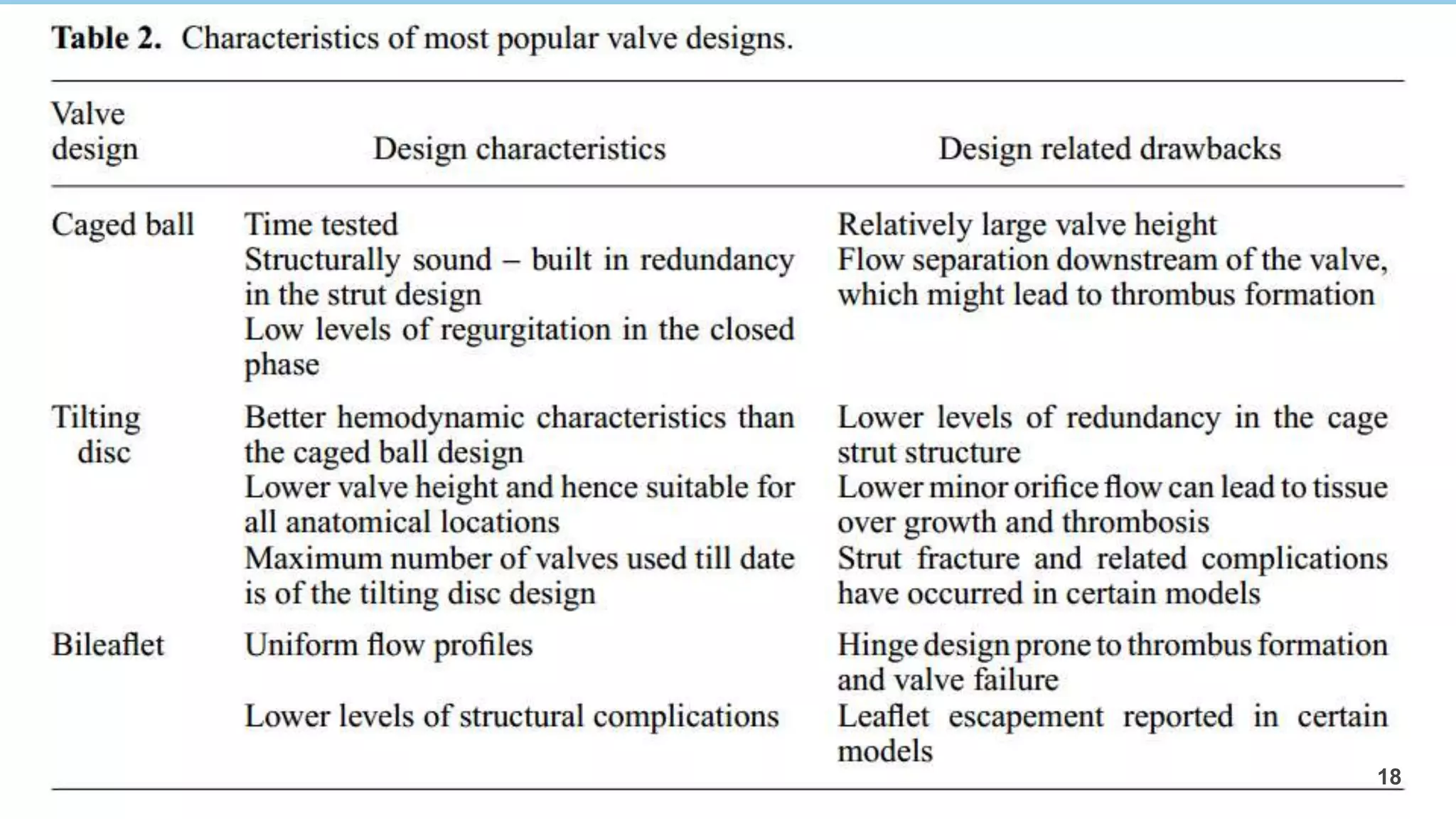
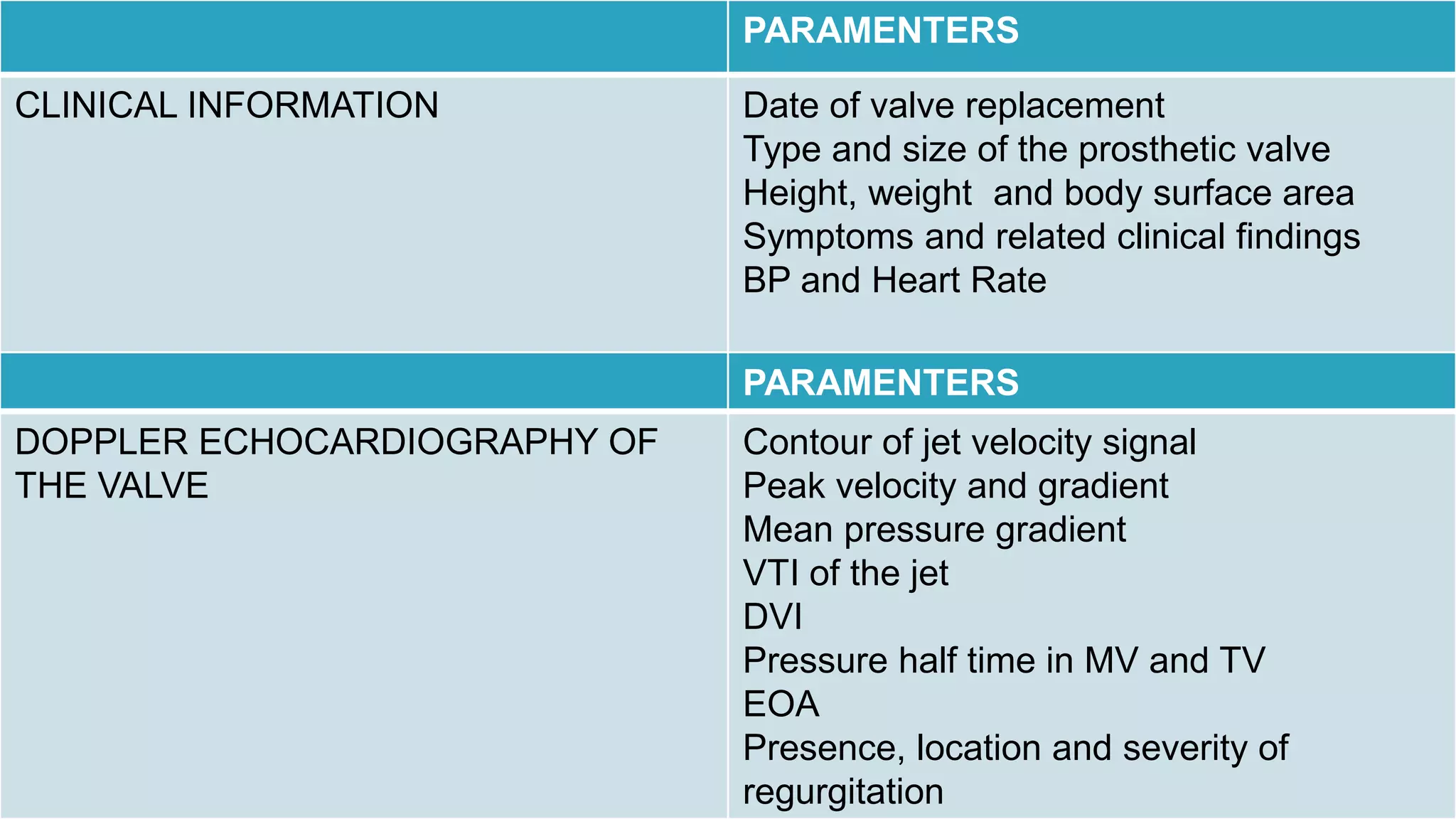
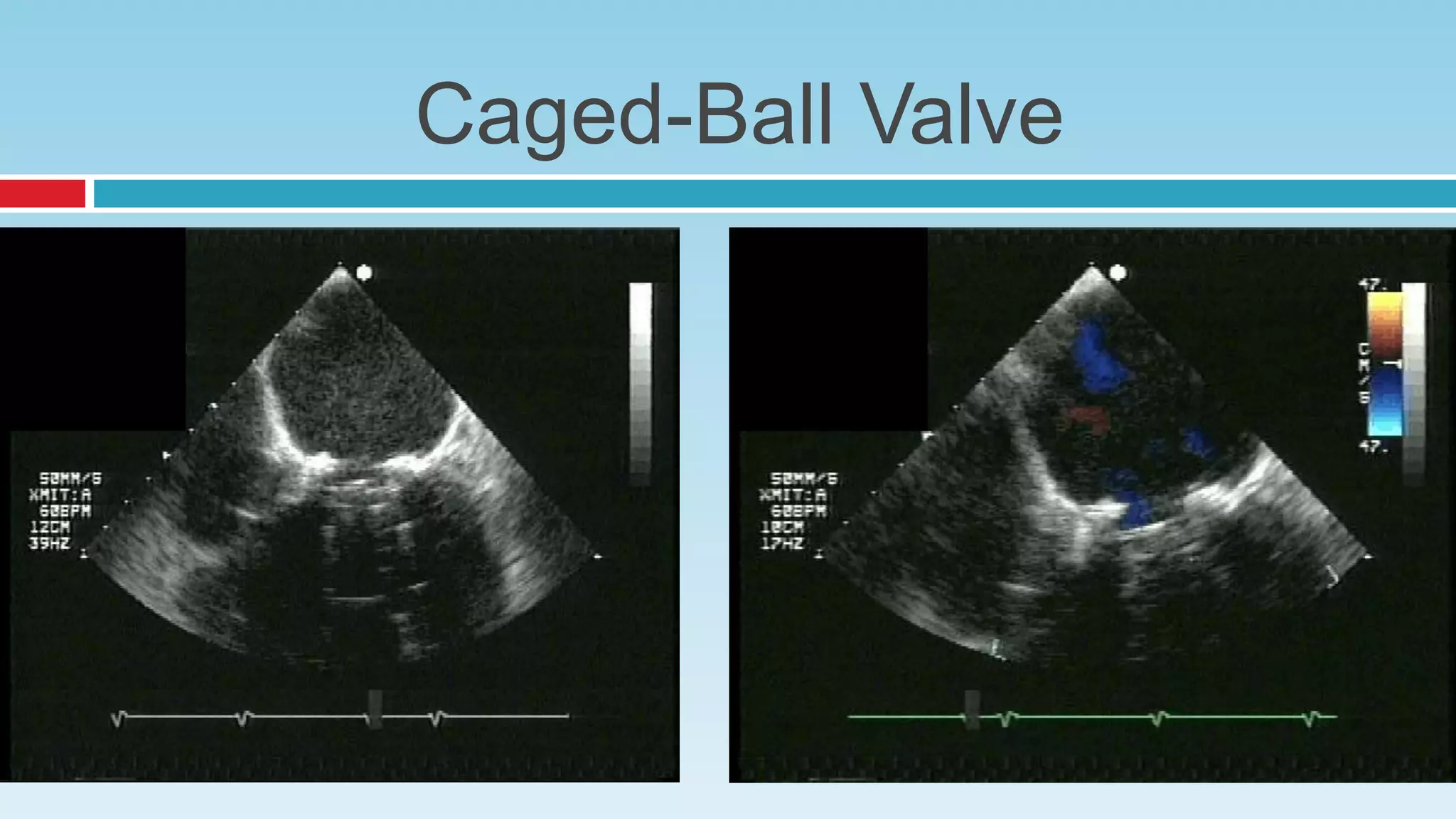
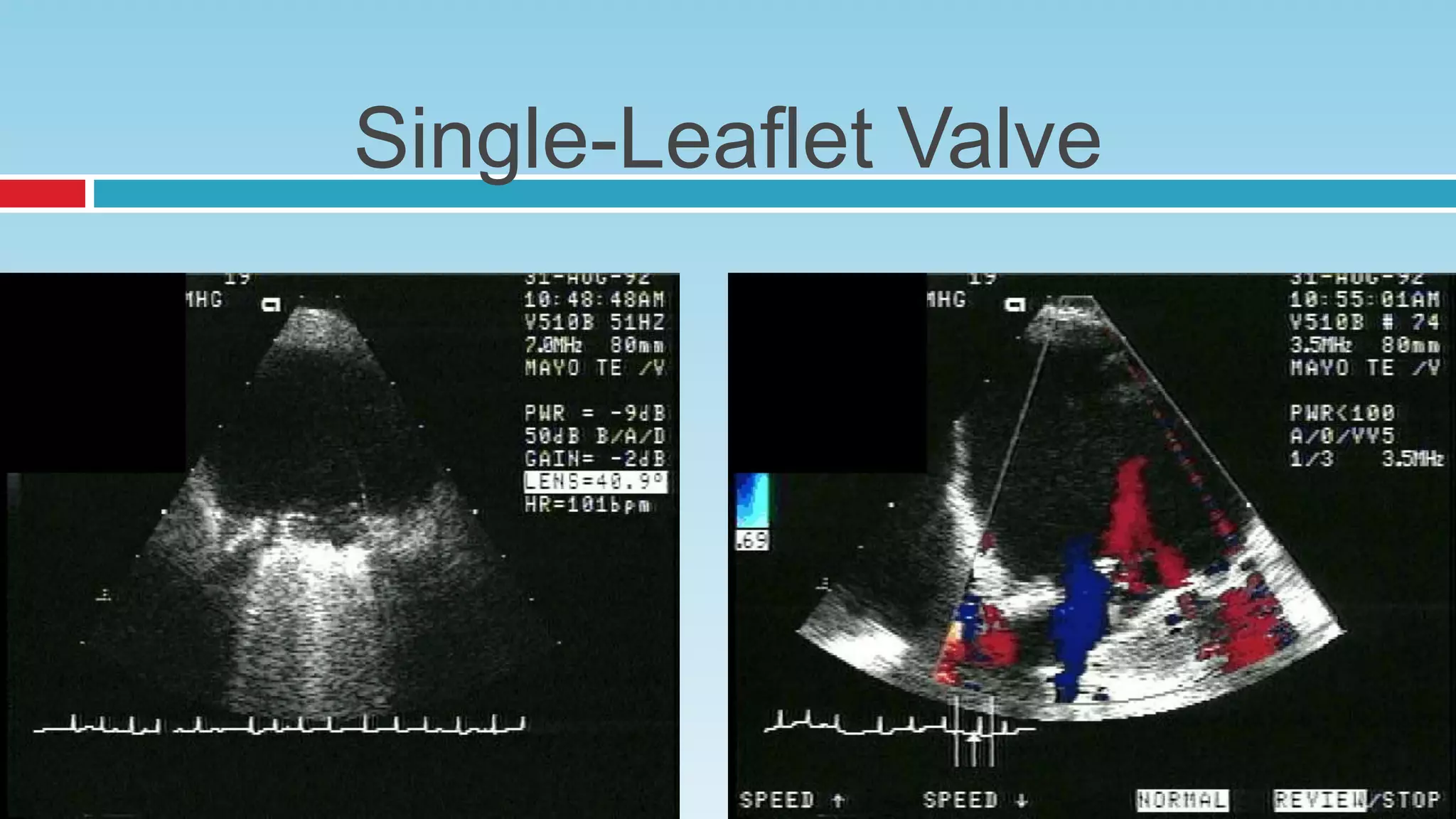
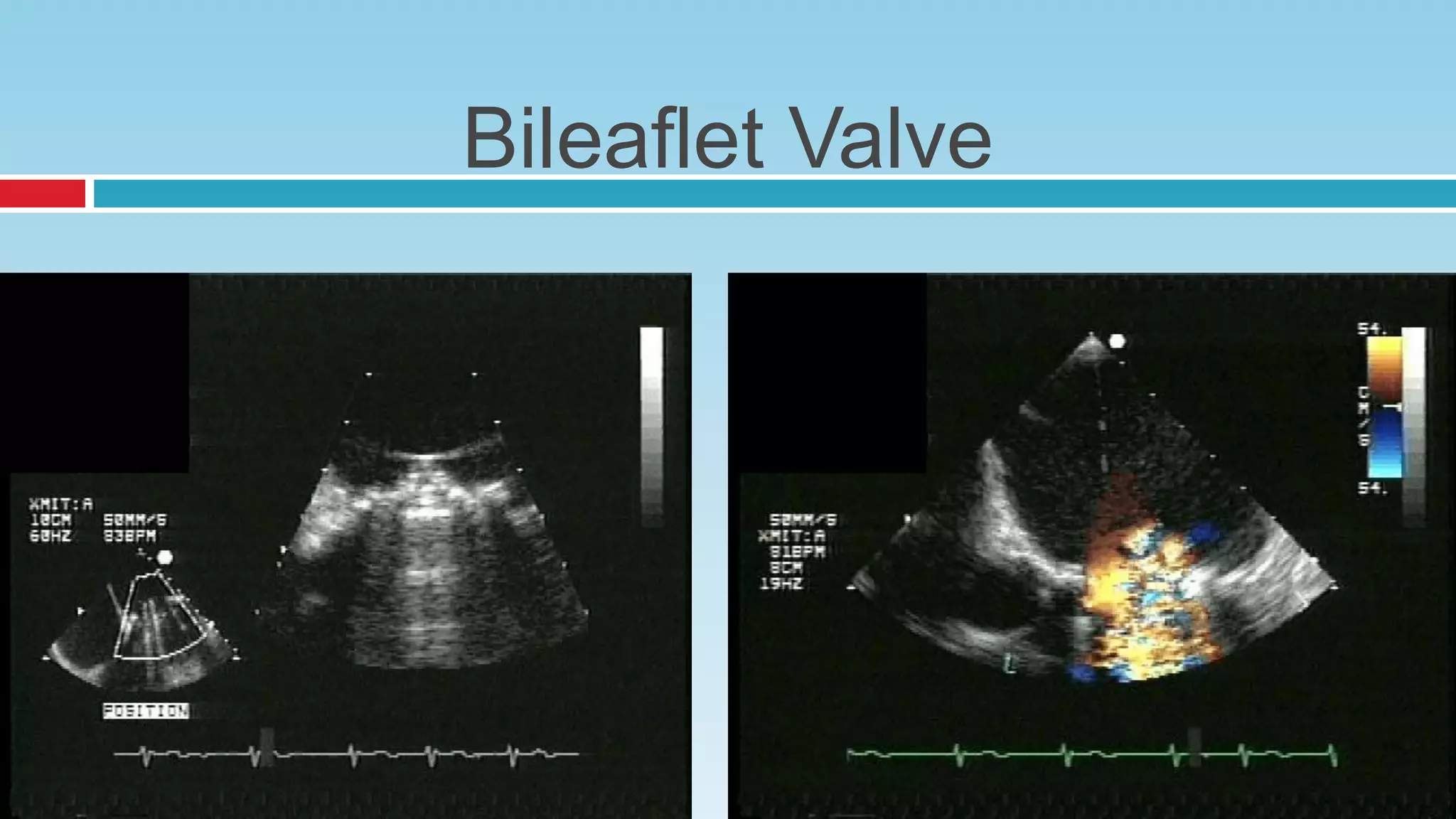
The document discusses different types of mechanical heart valves that have been developed over time to replace dysfunctional natural heart valves. It describes early valve designs like the ball-and-cage Starr-Edwards valve and the tilting disc Bjork-Shiley valve. More modern bileaflet valves are also discussed. The key materials used in heart valves include metals for strength as well as pyrolytic carbon and polymers which are durable and promote blood compatibility. Researchers continue working to improve valve lifespan, reduce risk of blood clots, and develop less invasive implantation methods.