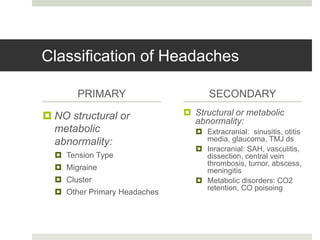
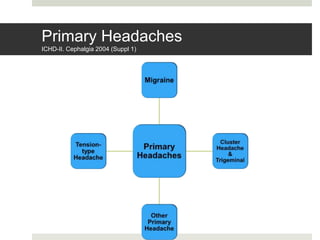
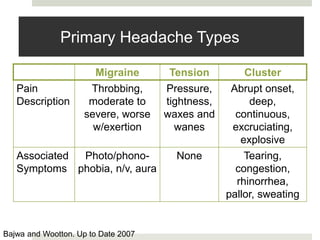
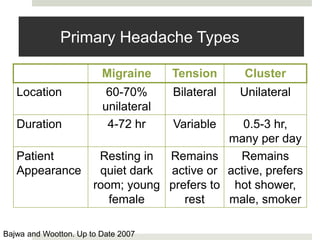
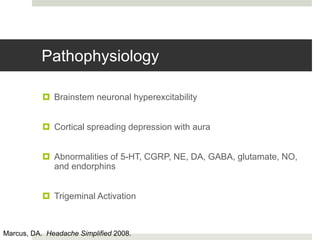
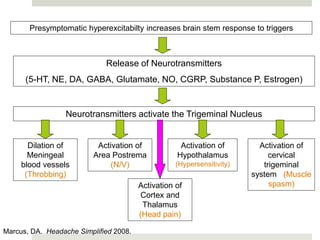
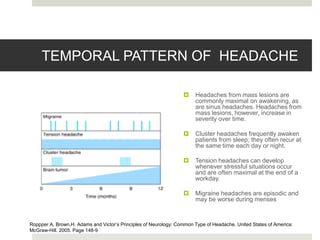
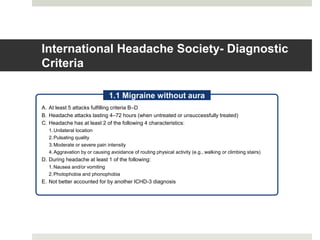
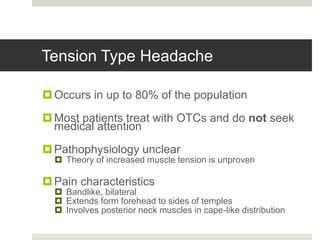
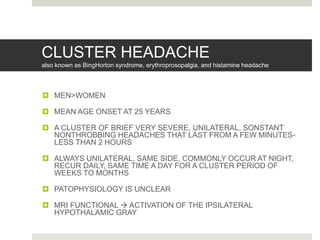
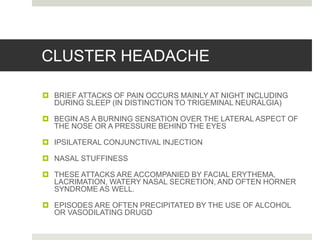
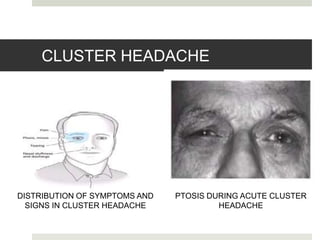
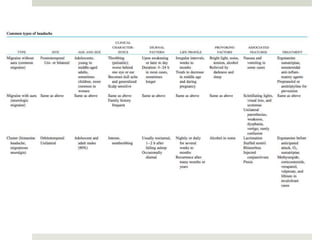
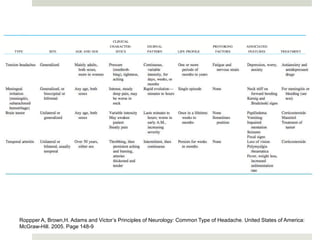
Primary headaches are caused by traction, inflammation or vascular changes affecting pain-sensitive structures in the head or neck. They include migraines, tension headaches and cluster headaches. Migraines typically cause moderate to severe throbbing pain that is worsened by activity along with nausea, photophobia and phonophobia. They are often relieved by sleep, vomiting or pressing on the temporal artery. Tension headaches cause mild to moderate non-pulsing pain that does not worsen with activity. Cluster headaches are characterized by severe, explosive pain around one eye and are associated with tearing and congestion.