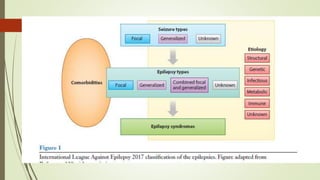
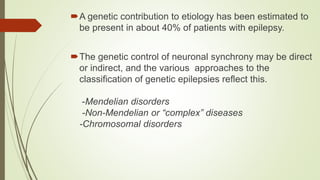
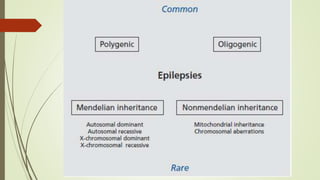
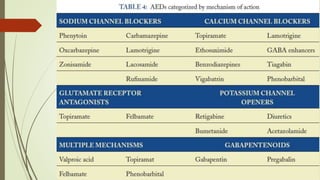
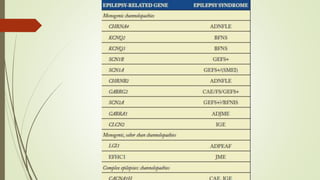
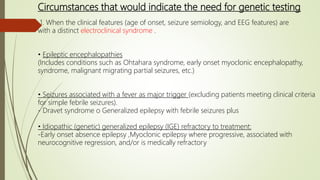
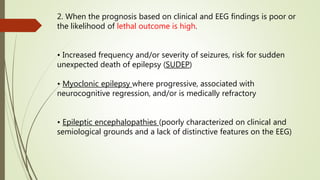
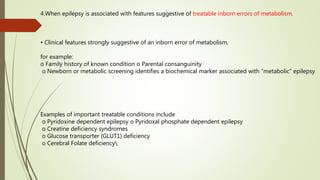
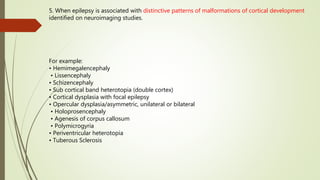
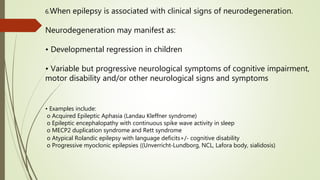
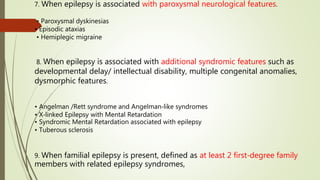
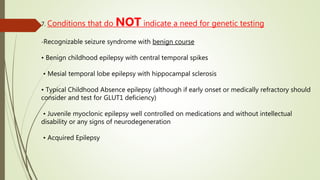
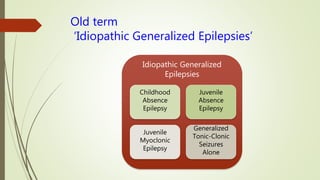
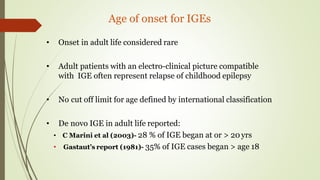
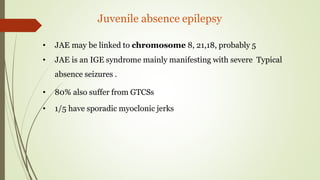
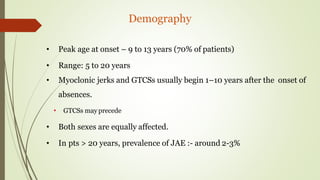
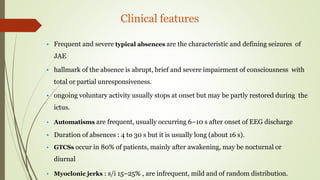
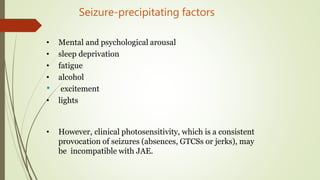
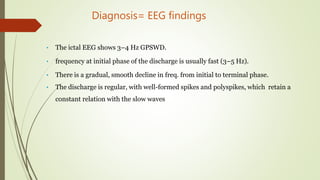
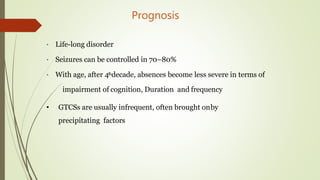
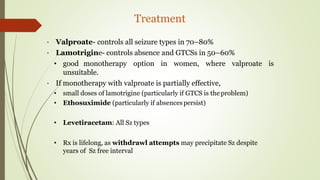
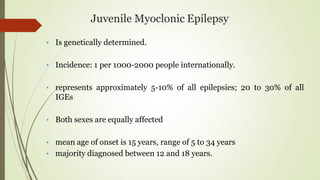
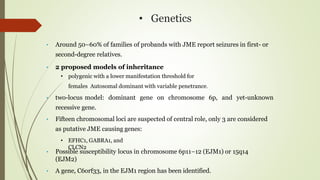
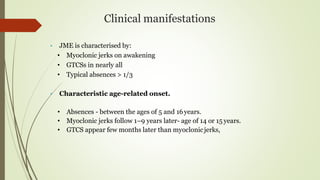
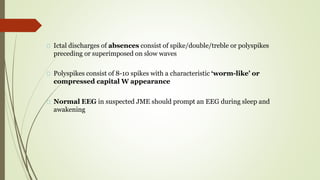
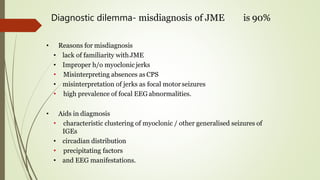
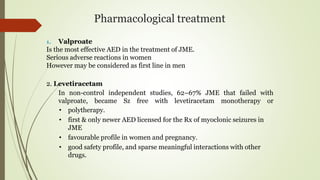
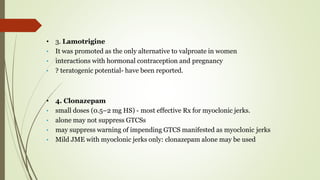
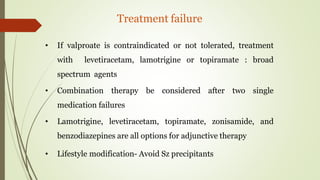
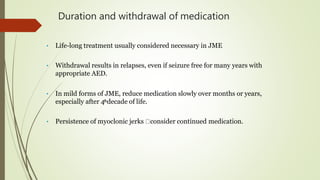
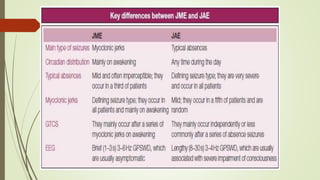
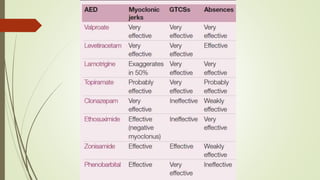
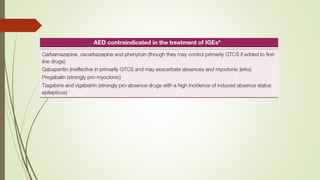
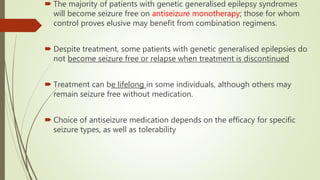
This document provides information on genetic epilepsy and juvenile myoclonic epilepsy. It defines epilepsy and describes its various classifications including idiopathic, symptomatic and cryptogenic epilepsy. Juvenile myoclonic epilepsy is discussed in detail, including its genetics, clinical manifestations such as myoclonic jerks and absence seizures, diagnosis through EEG findings, and treatment options involving anti-seizure medications. Circumstances for genetic testing in epilepsy cases are outlined.