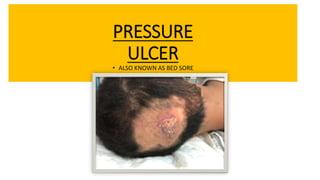
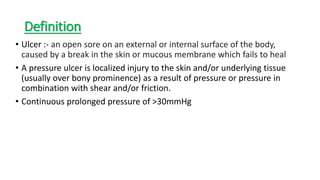
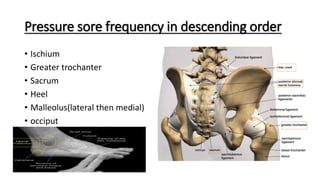
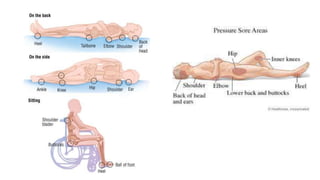
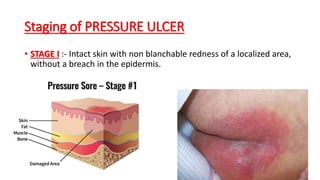
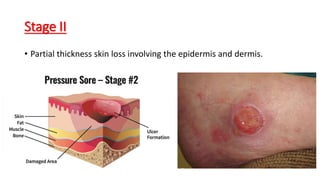
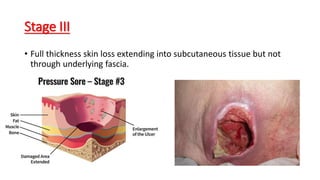
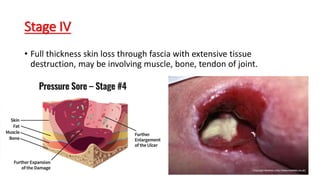
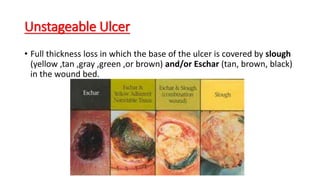
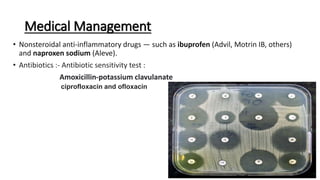
The document discusses the importance of bed making and the prevention and management of pressure ulcers in ICU patients. It details risk factors, clinical features, staging, and collaborative care approaches, including nursing and medical management strategies. The need for regular assessment and repositioning of patients to prevent bed sores is emphasized, along with the implementation of specific prevention techniques.