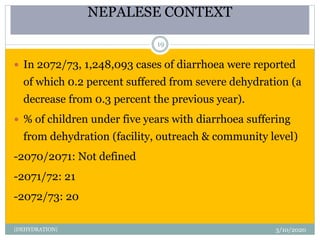
The presentation covers dehydration, detailing its definition, clinical features, causes, and treatment approaches, as well as specific data on dehydration in the Nepalese context. Key objectives include understanding risk factors and signs of dehydration and providing first aid management techniques. The ABCDE approach for triaging patients is emphasized for effective emergency management.