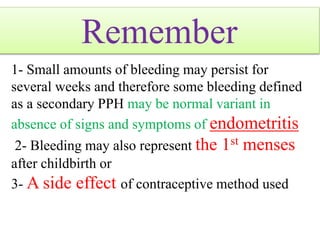
1. Secondary postpartum hemorrhage (PPH) is defined as excessive or fresh bleeding from the vagina between 24 hours and 12 weeks after childbirth.
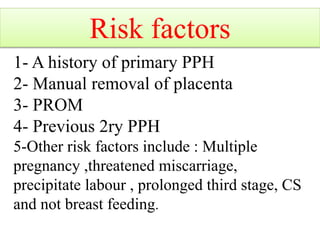
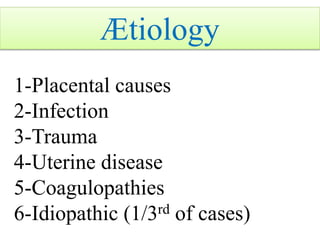
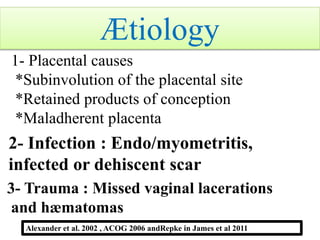
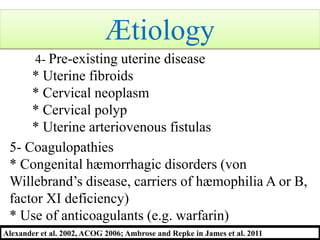
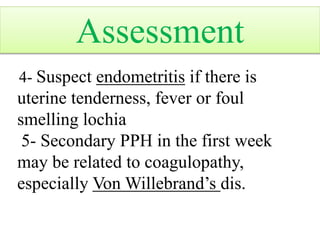
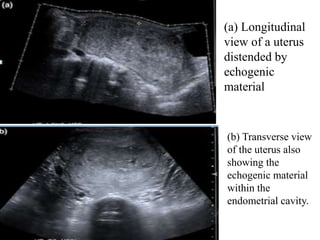
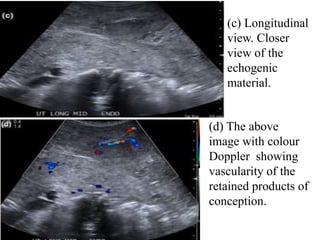
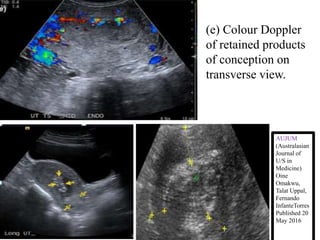
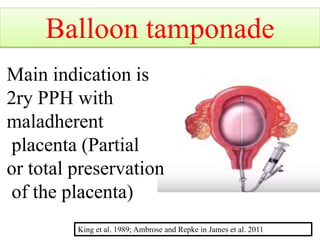
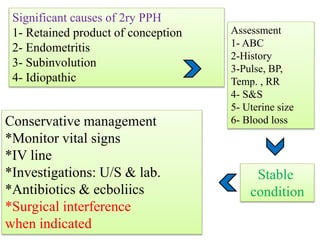
2. Causes of secondary PPH include retained placenta, infection, trauma, uterine abnormalities, and coagulation disorders.
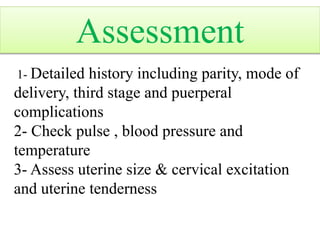
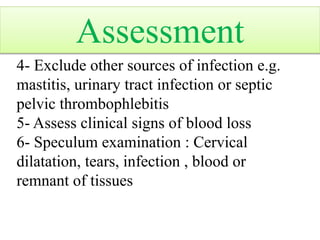
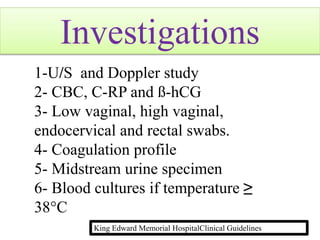
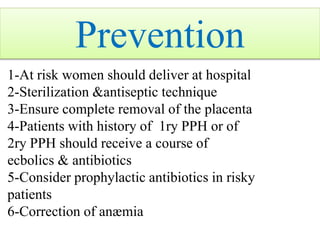
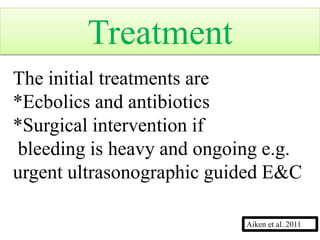
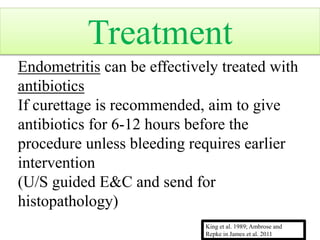
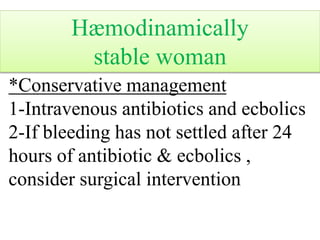
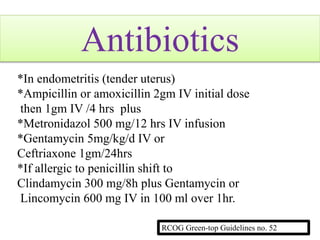
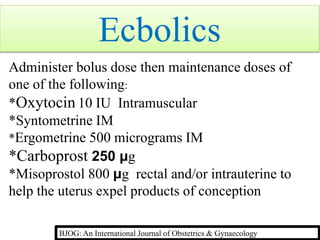
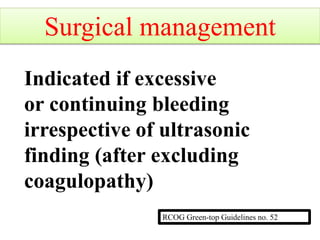
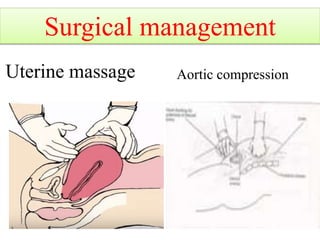
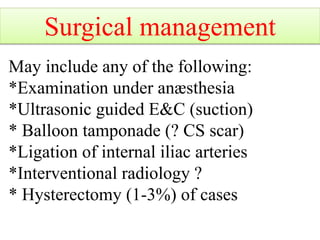
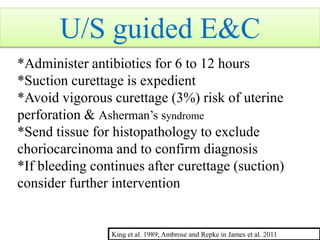
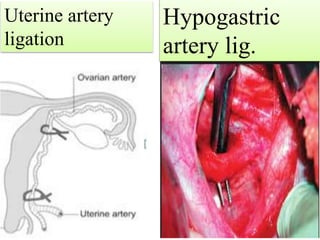
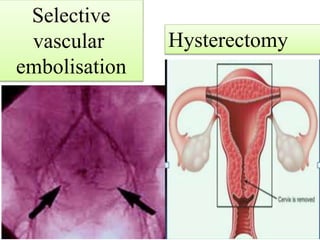
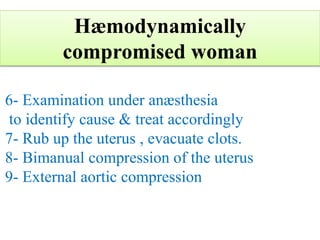
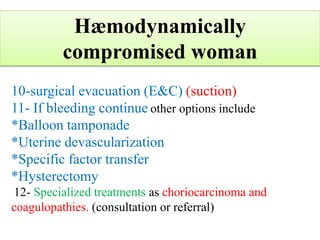
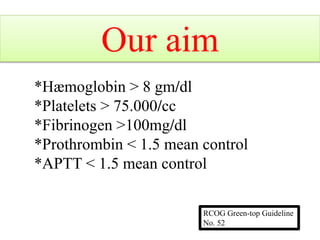
3. Assessment involves vital signs, uterine size, cervical examination, and lab tests. Conservative management includes antibiotics, uterotonic drugs, and surgical intervention if bleeding continues.
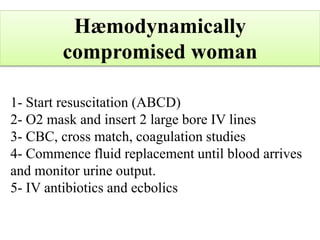
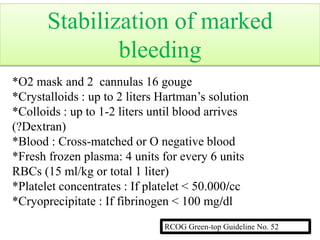
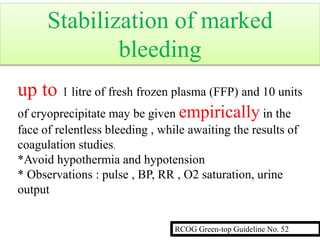
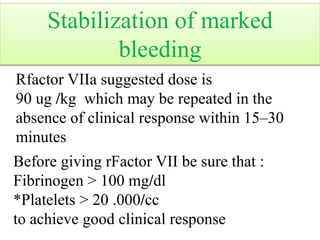
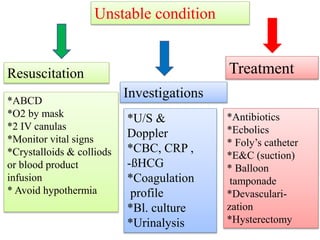
4. For unstable patients, resuscitation is prioritized with IV fluids, blood products, and treating the underlying cause. Hysterectomy may be required in some severe cases.