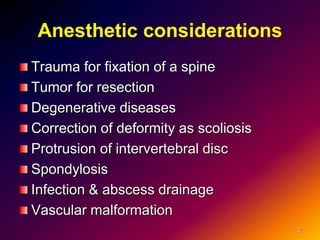
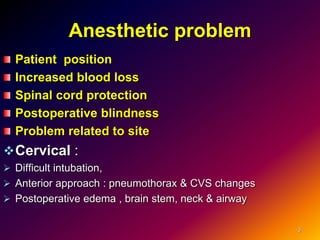
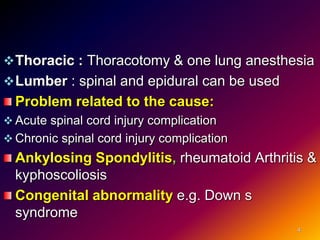
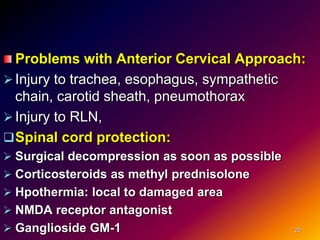
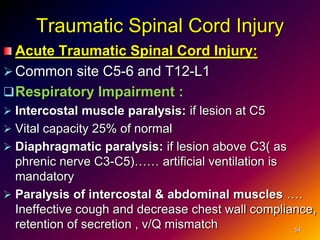
1. Anesthesia for spine surgery presents several challenges including patient positioning, increased blood loss, and spinal cord protection.
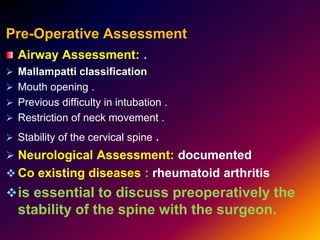
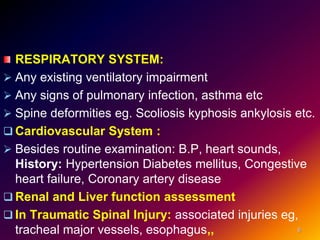
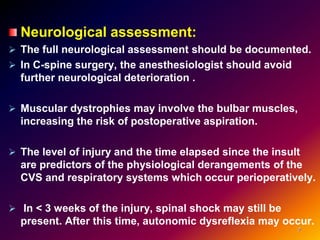
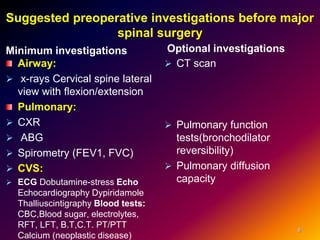
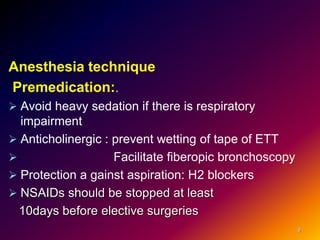
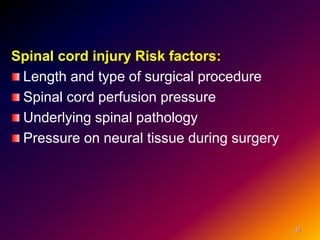
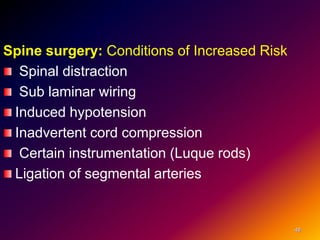
2. Pre-operative assessment focuses on airway evaluation, neurological and cardiovascular status, and determining risk factors for complications.
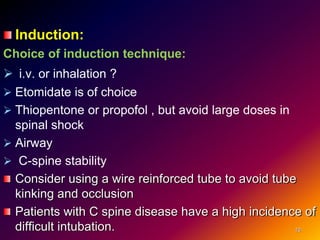
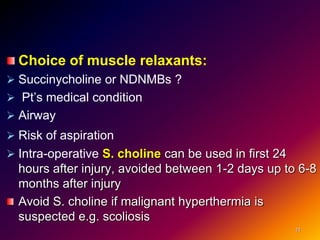
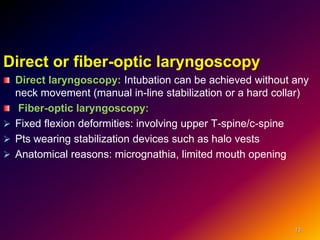
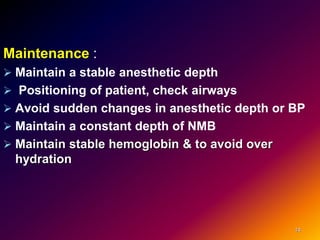
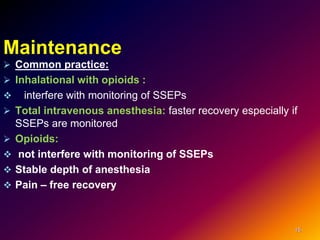
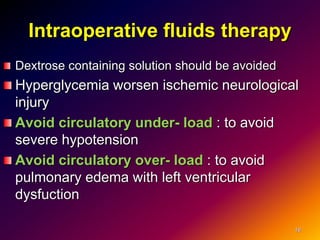
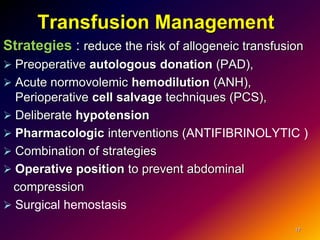
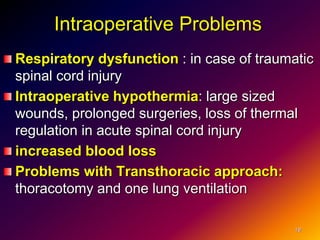
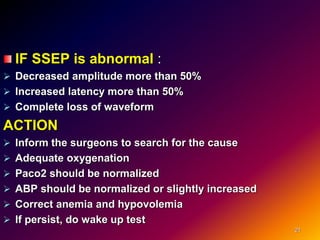
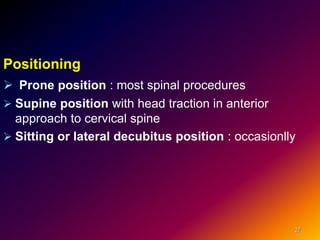
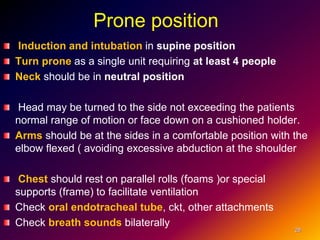
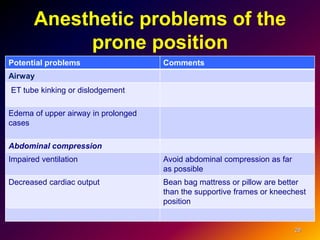
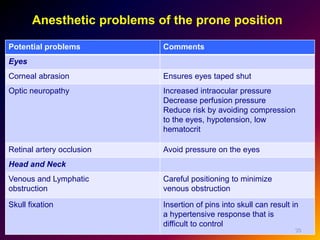
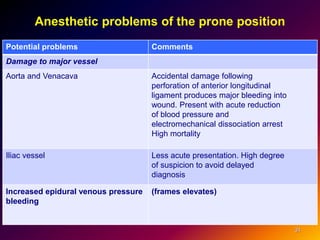
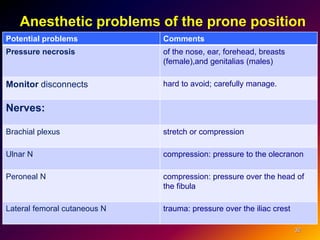
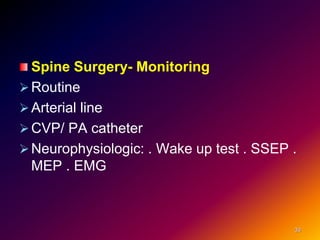
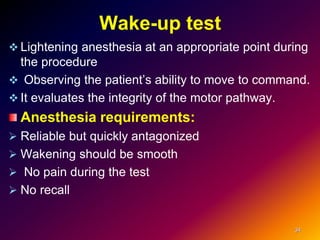
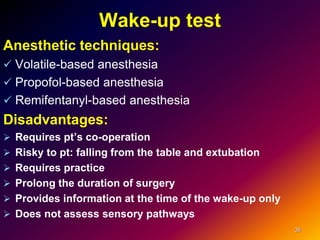
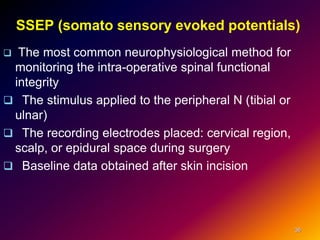
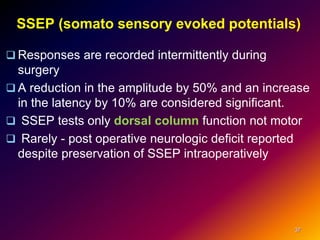
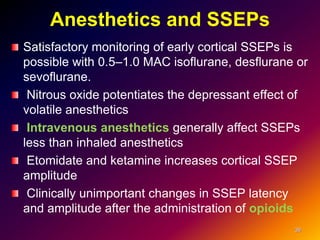
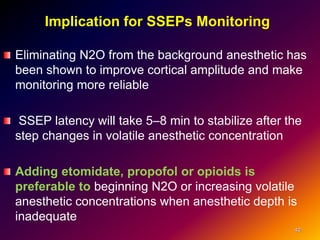
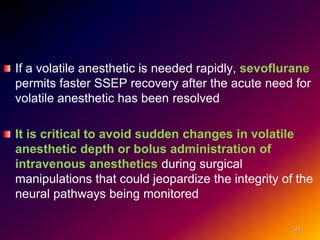
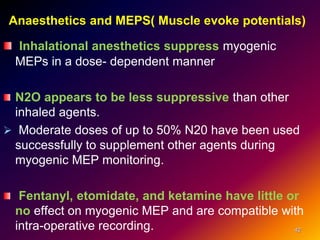
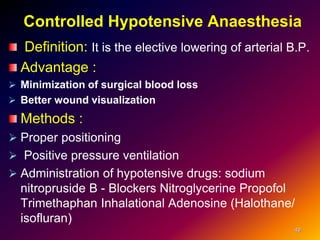
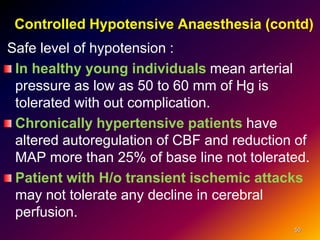
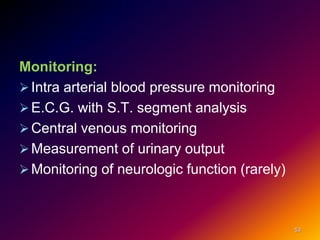
3. During surgery, careful positioning, maintenance of stable anesthesia and hemodynamics, and monitoring for changes like abnormal SSEPs are important considerations.
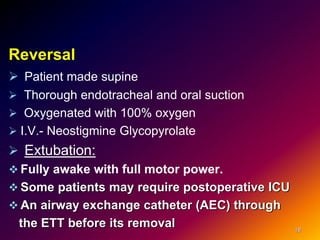
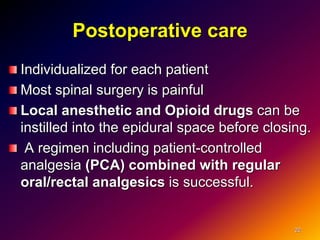
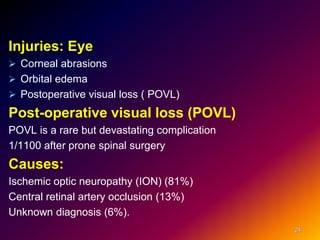
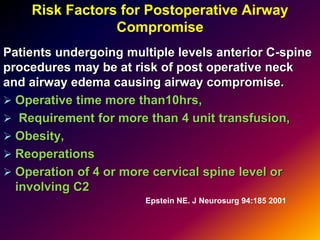
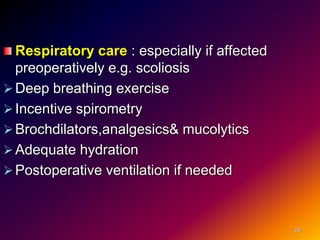
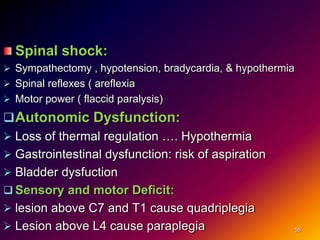
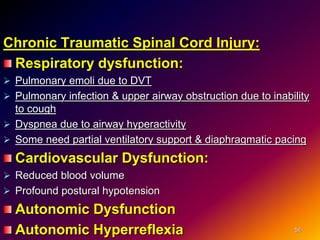
4. Post-operative care involves managing pain, monitoring for complications, and addressing issues like respiratory function, neck edema, and injury risks from prolonged prone positioning.