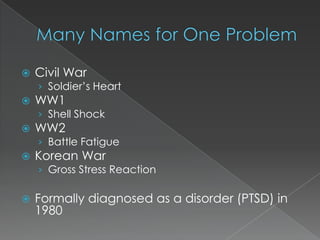
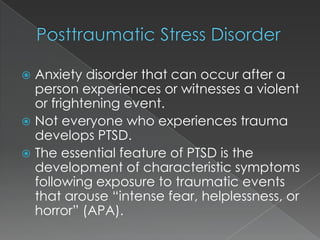
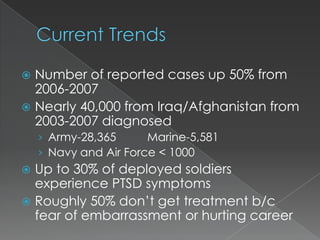
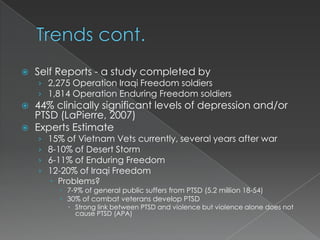
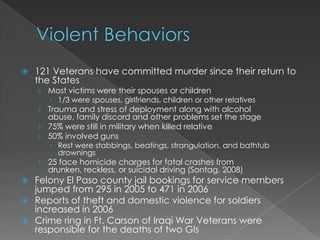
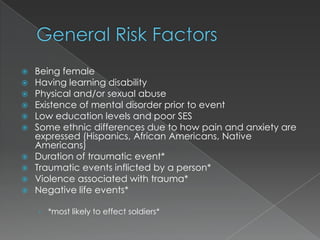
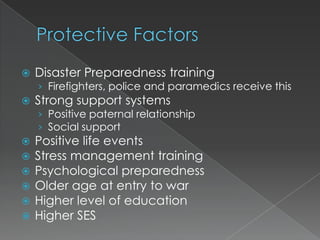
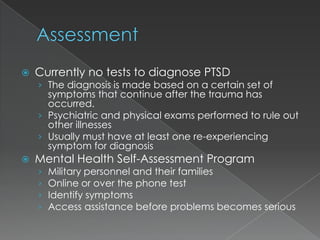
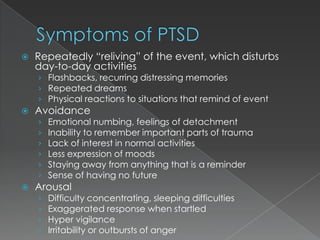
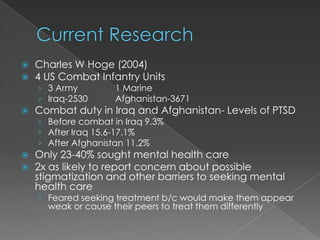
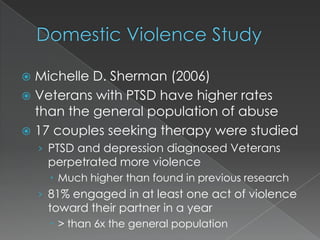
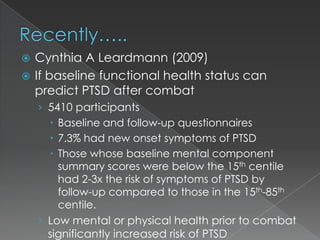
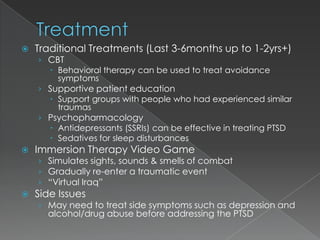
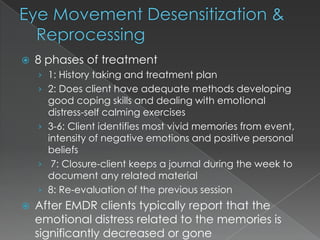
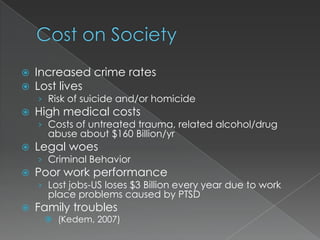
The document discusses post-traumatic stress disorder (PTSD) in military veterans and service members. It provides a brief history of PTSD and how it has been diagnosed over time. Statistics are presented showing high rates of PTSD among recent veterans deployed to Iraq and Afghanistan, with only about half seeking treatment due to fears of stigma. Risk factors, symptoms, treatments and prevention strategies are outlined. The impacts of untreated PTSD include increased crime, substance abuse, domestic violence, broken relationships and poor work performance.