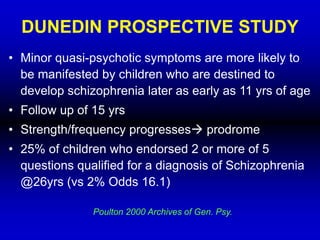
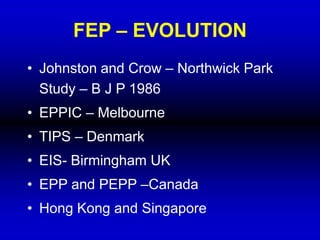
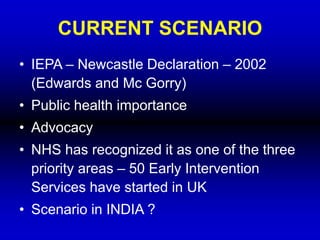
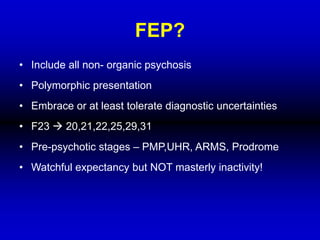
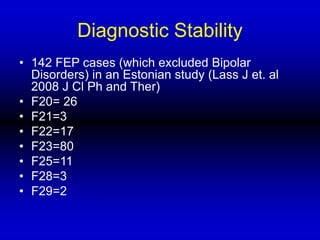
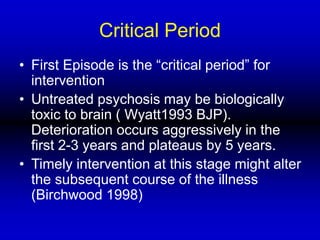
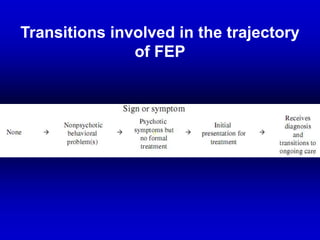
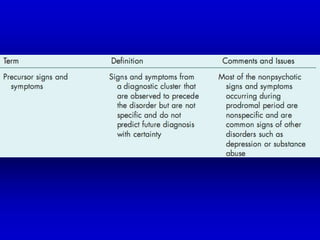
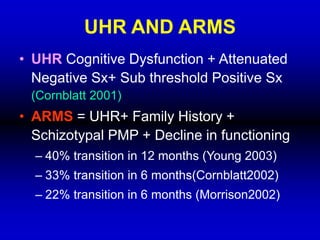
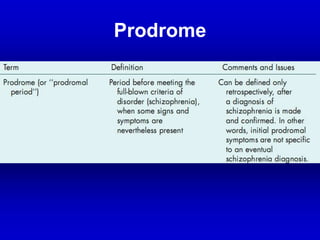
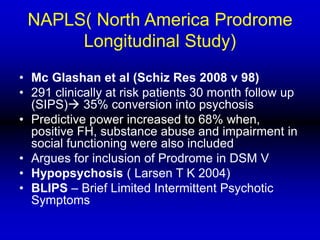
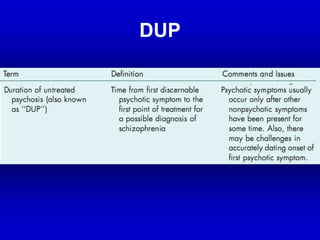
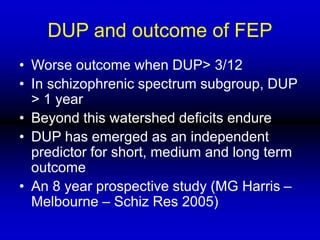
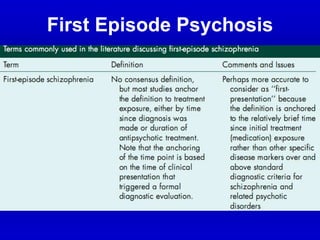
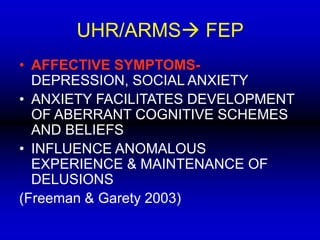
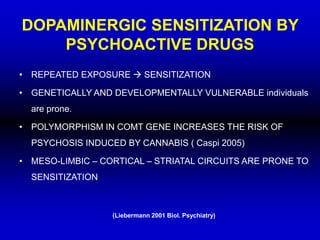
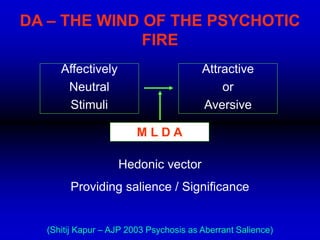
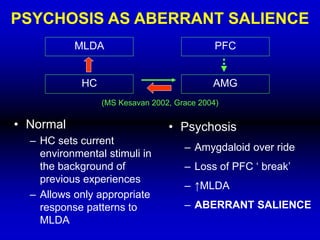
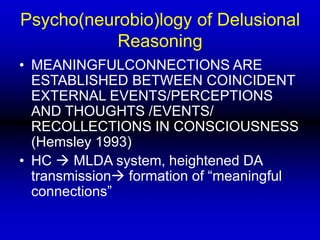
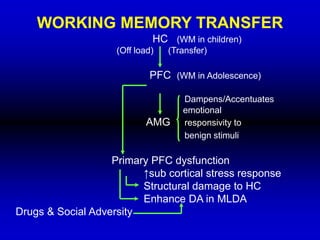
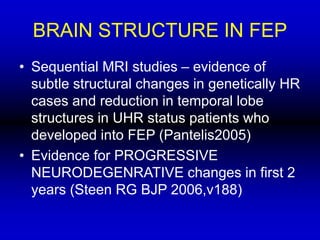
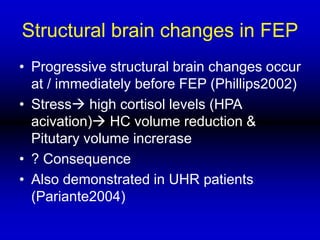
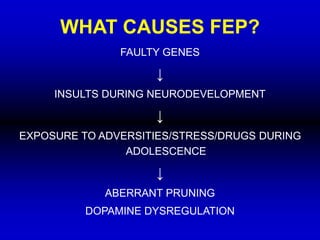
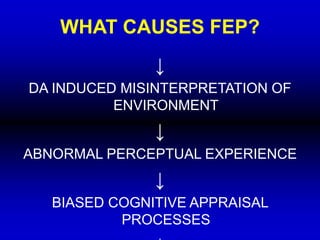
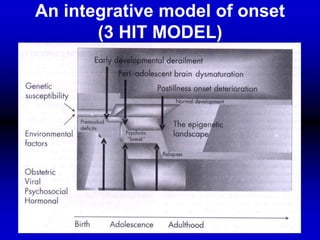
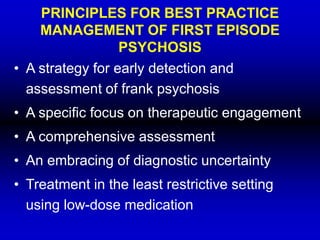
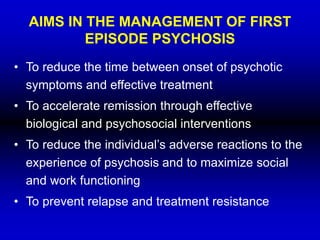
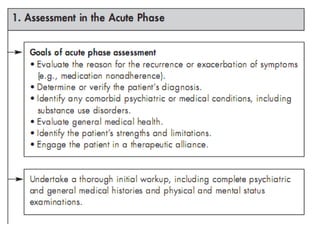
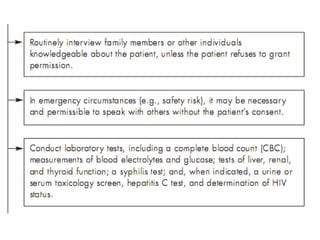
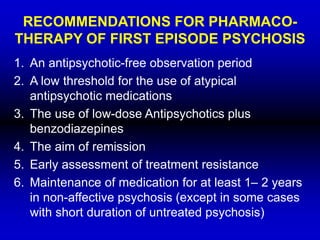
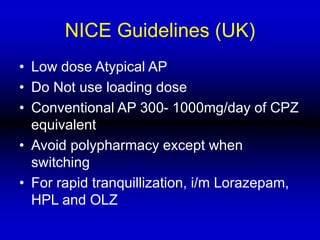
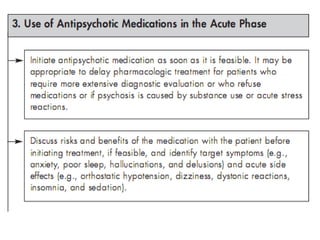
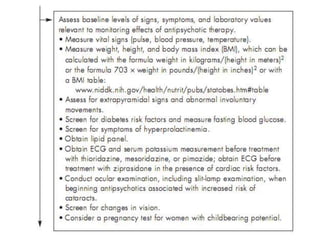
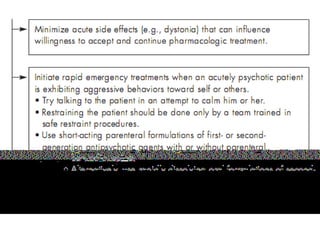
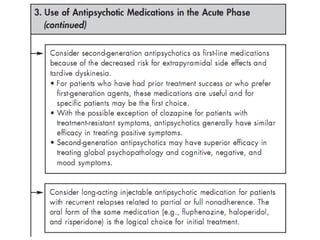
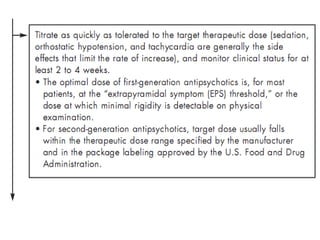
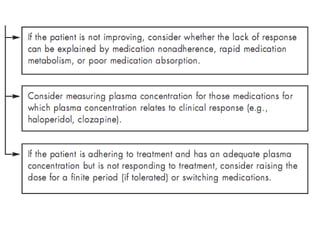
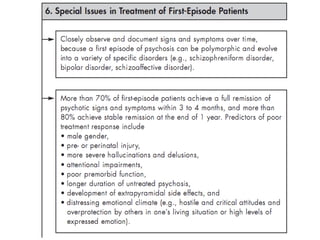
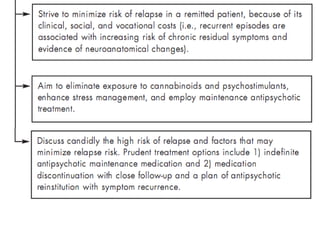
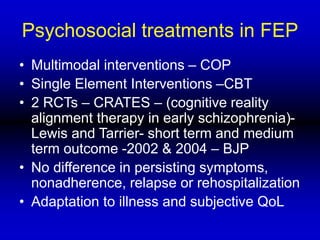
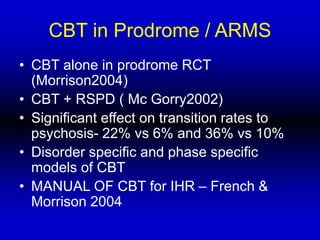
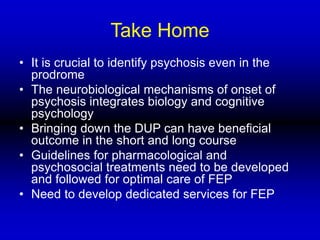
This document provides an overview of first episode psychosis (FEP), including its history, concepts, neurobiology, assessment, management, and guidelines. It discusses the prodromal phase and periods like the duration of untreated psychosis. Studies show minor quasi-psychotic symptoms can occur up to 11 years before schizophrenia onset. Prodromal states like the ultra-high risk and attenuated risk mental states are described, which have high transition rates to psychosis. Dopamine dysregulation and social and substance use factors are implicated in the onset of FEP. Assessment and management should follow a low-dose approach with psychosocial support to reduce time to treatment and maximize functioning.