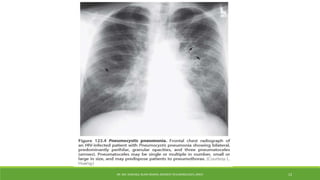
Pneumocystis pneumonia is a serious fungal infection caused by Pneumocystis jirovecii that mainly affects those with weakened immune systems, such as those with HIV/AIDS or those taking immunosuppressive medications. It presents with fever, cough, and shortness of breath. Diagnosis involves microscopic examination of respiratory samples or biopsy to detect the fungus. Chest imaging typically shows bilateral infiltrates. Treatment is primarily trimethoprim-sulfamethoxazole administered for 21 days along with corticosteroids for more severe cases.