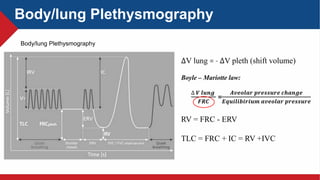
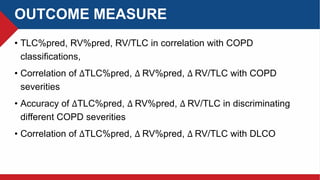
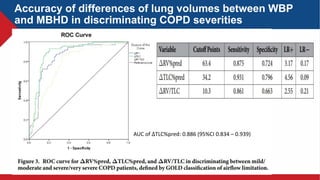
This study analyzes lung volume measurements in COPD patients using whole body plethysmography (WBP) and multi-breath helium dilution (MBHD) methods. The results demonstrate that differences in lung volumes between WBP and MBHD correlate with COPD severity, with WBP showing significantly higher values than MBHD. The findings suggest that these measurement techniques can effectively differentiate the levels of airflow obstruction and gas trapping in COPD patients.