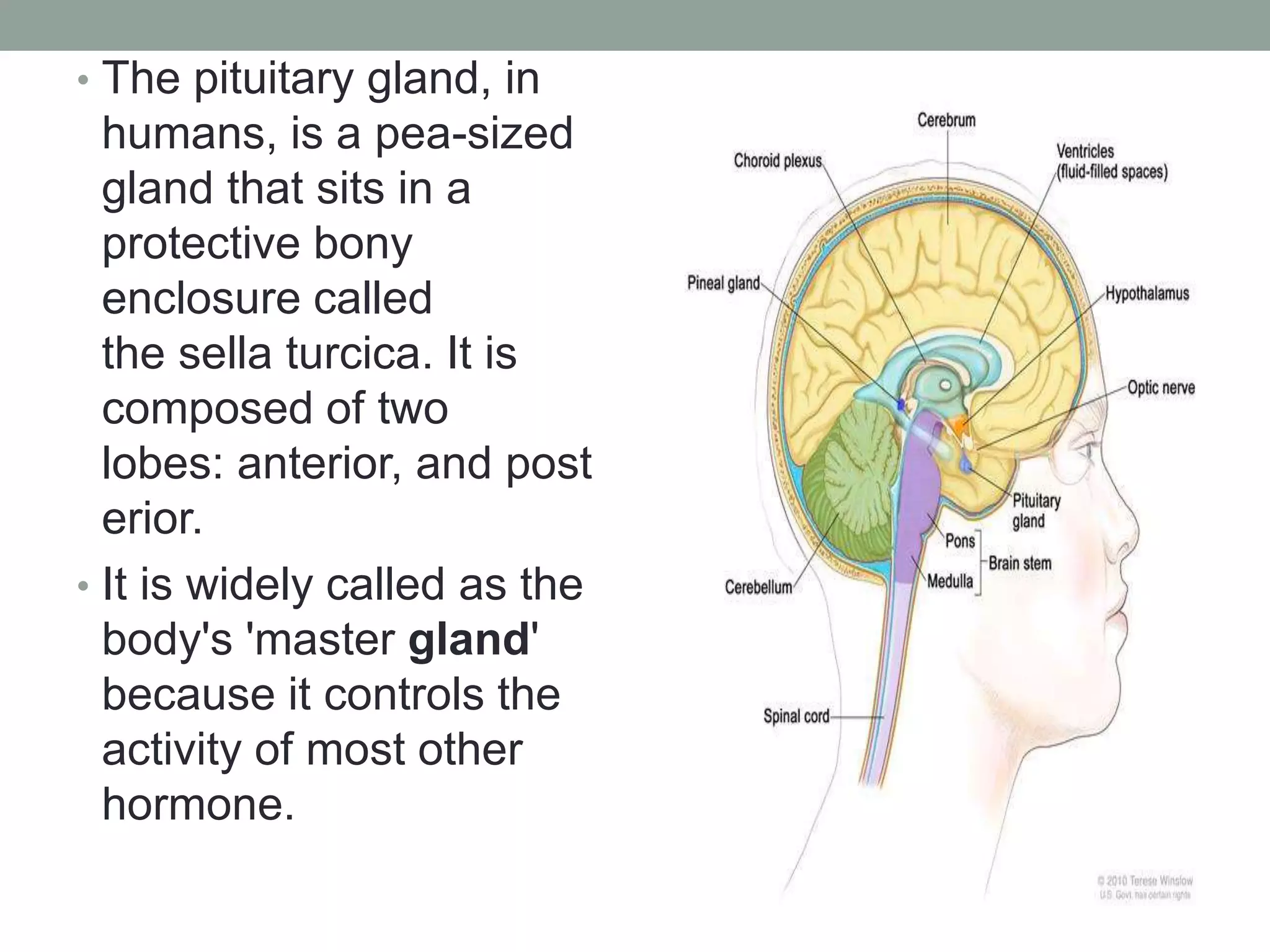
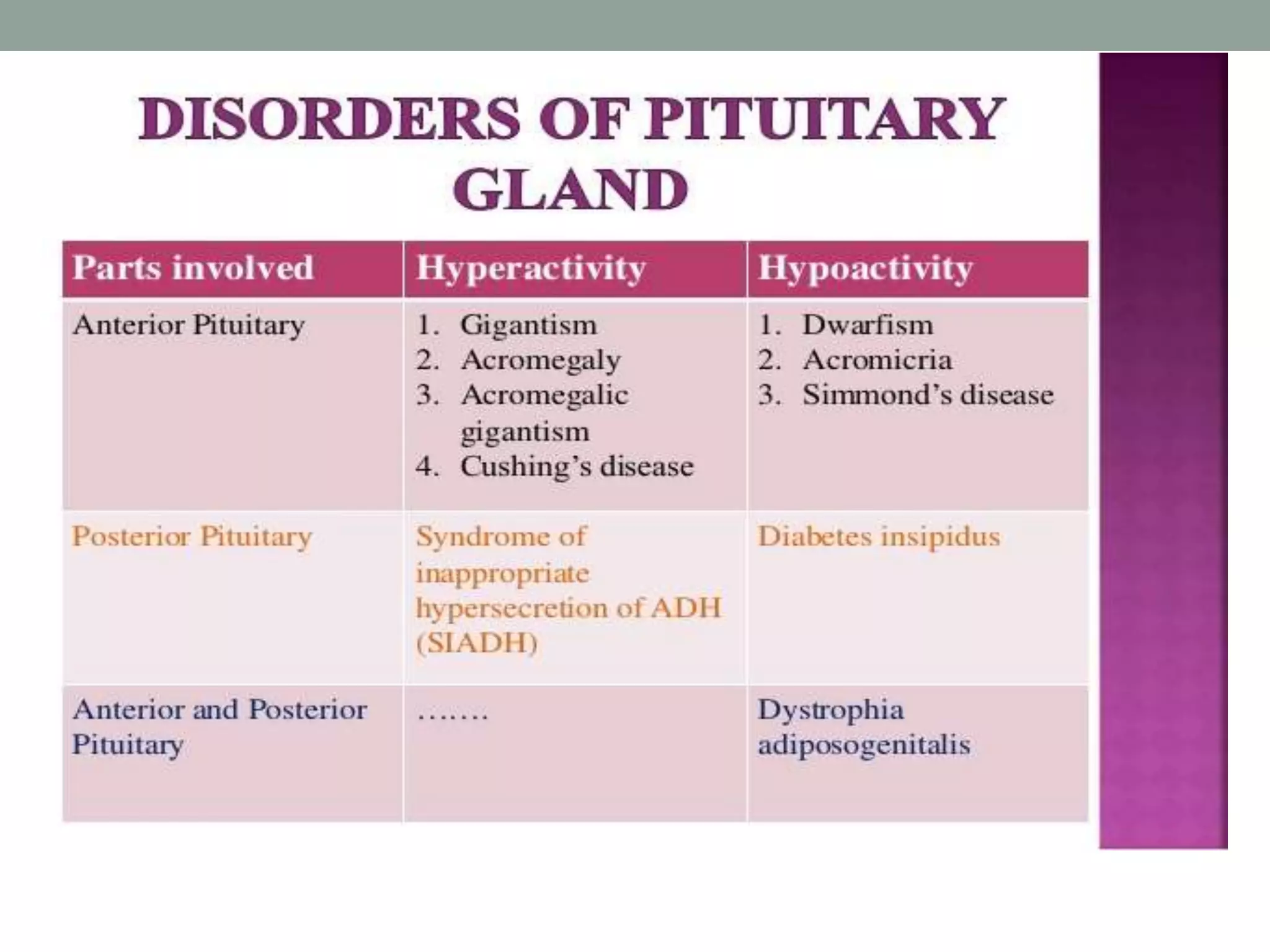
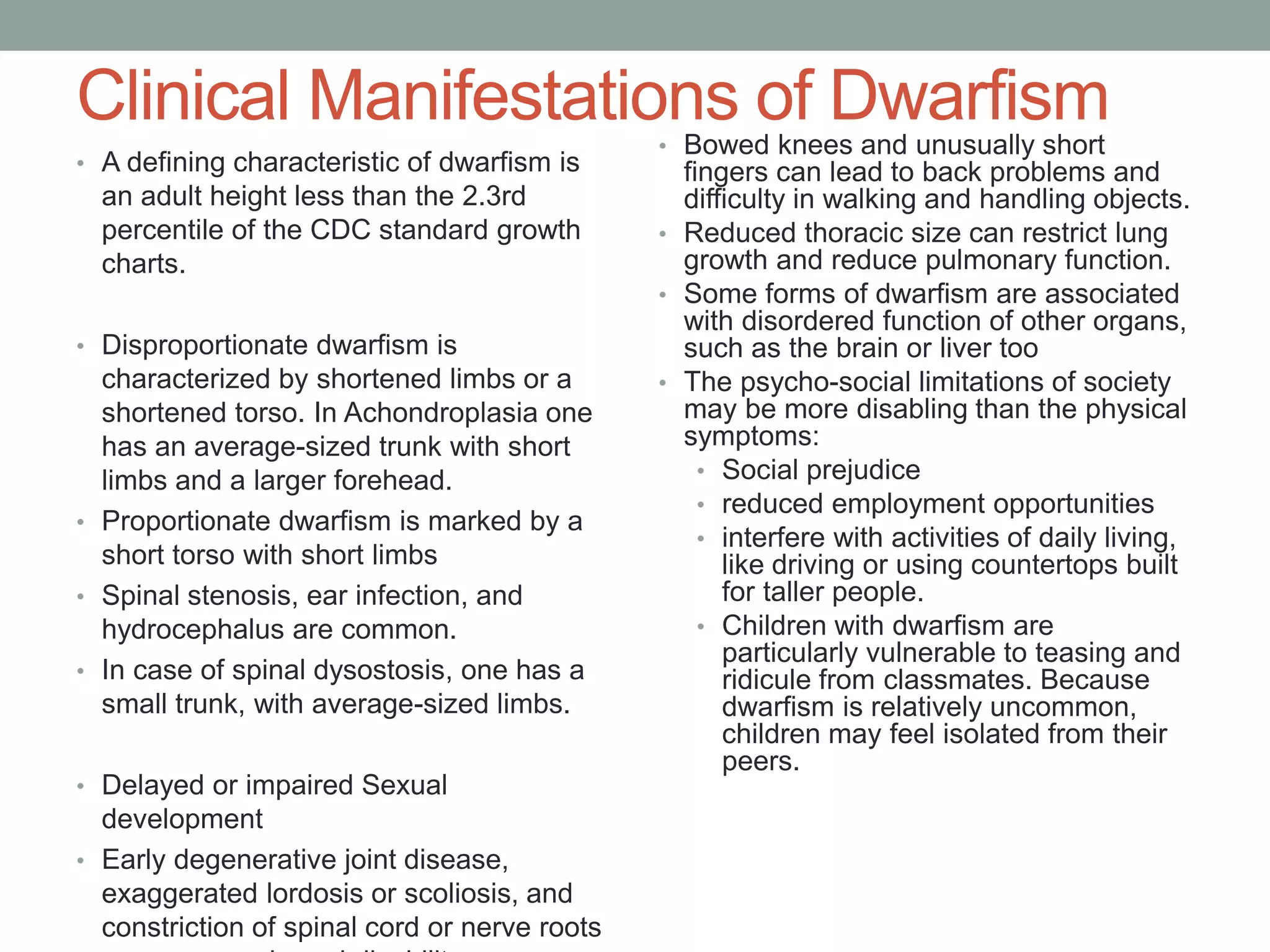
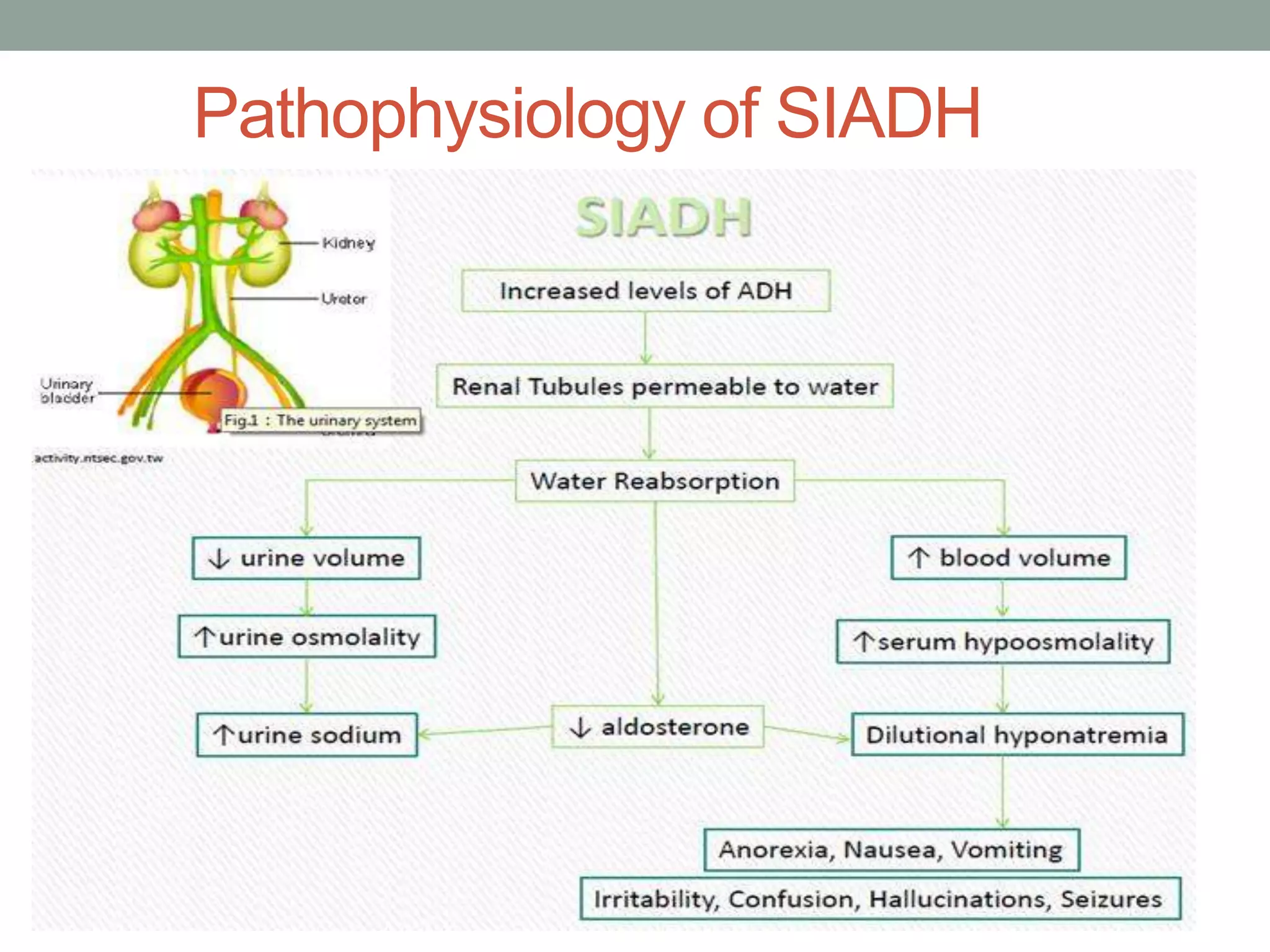
The pituitary gland sits at the base of the brain and controls many other glands. Acromegaly is caused by excess growth hormone after growth plate closure, usually due to a pituitary adenoma. Complications include joint and bone problems, high blood pressure, diabetes, and increased cancer risk. Treatment involves surgery, medication, or radiation. Dwarfism is defined as adult height under 4'10" and has many causes and health issues. The pituitary also regulates water balance, and disorders like SIADH cause inappropriate antidiuretic hormone secretion leading to hyponatremia.