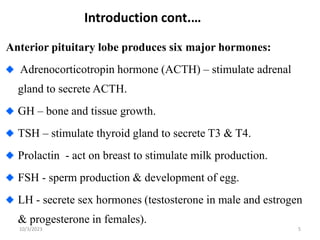
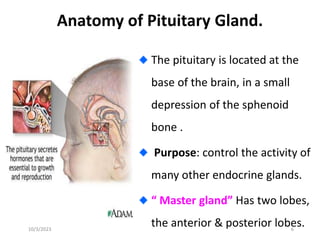
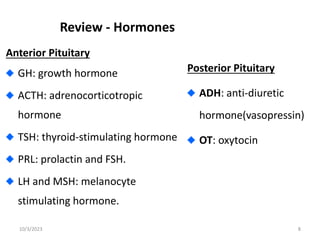
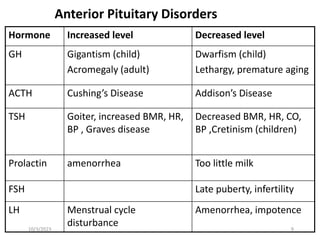
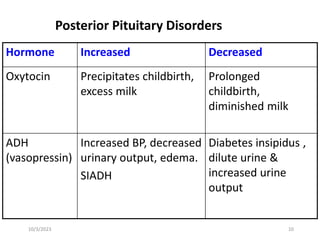
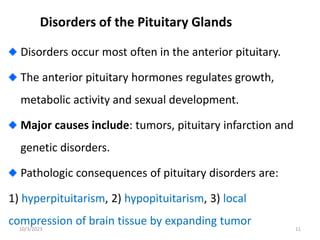
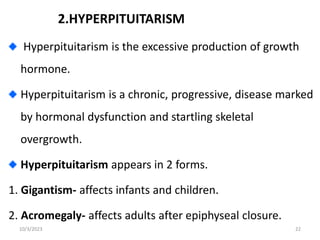
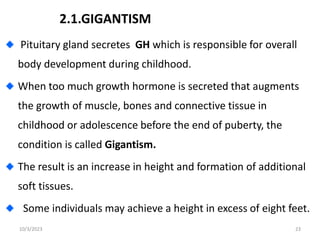
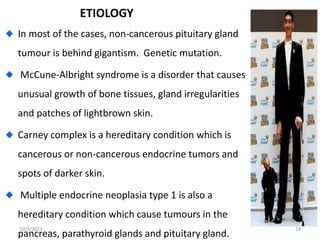
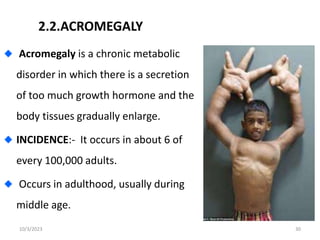
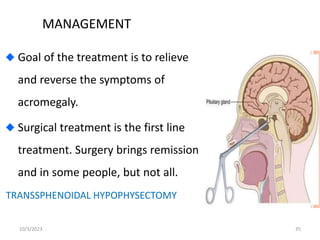
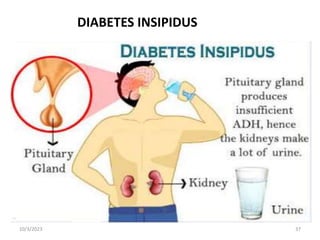
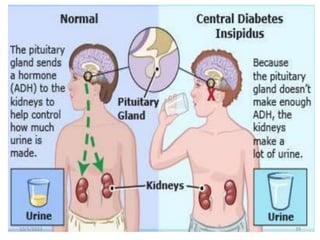
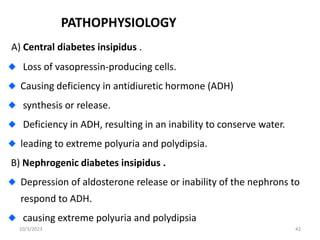
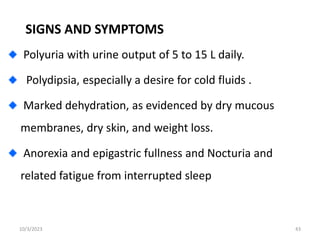
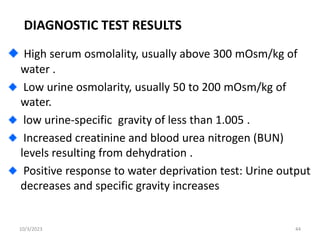
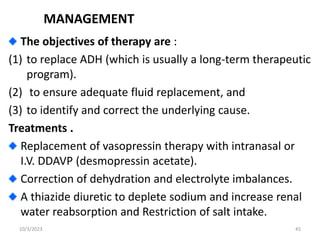
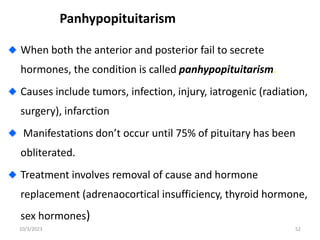
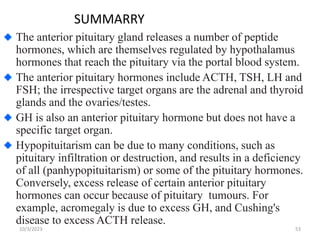
Pituitary disorders occur when there is too much or too little production of hormones by the pituitary gland. Some key pituitary disorders include hypopituitarism, hyperpituitarism, gigantism, acromegaly, and diabetes insipidus. Hypopituitarism is characterized by a loss of pituitary function and hormone deficiencies. Hyperpituitarism involves excessive hormone production and can manifest as gigantism in children or acromegaly in adults. Diabetes insipidus is caused by a deficiency or resistance to antidiuretic hormone, leading to excessive urination and thirst. These disorders are diagnosed through medical history, physical exams, imaging, and blood tests, and treatments aim to replace missing hormones