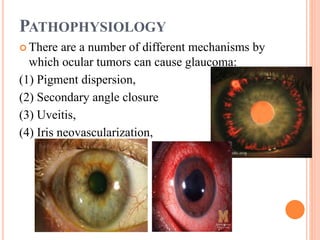
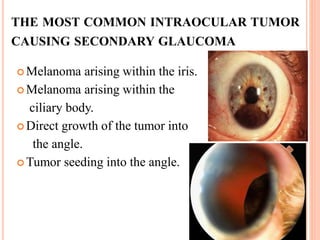
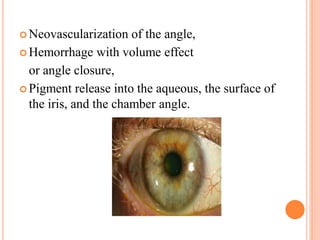
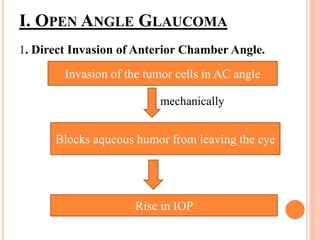
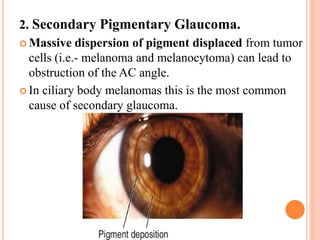
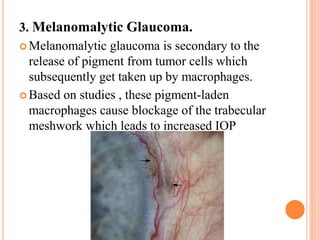
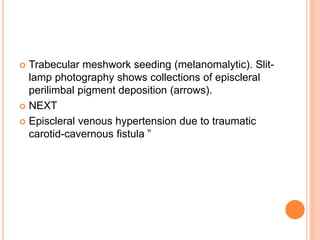
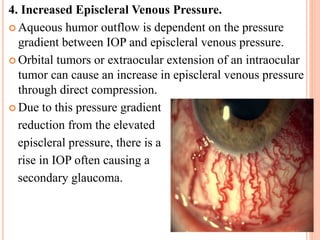
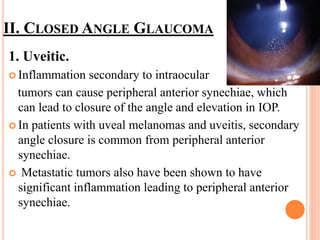
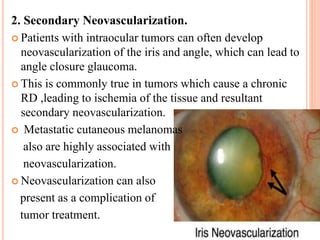
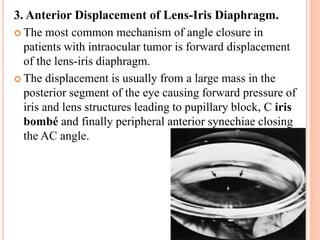
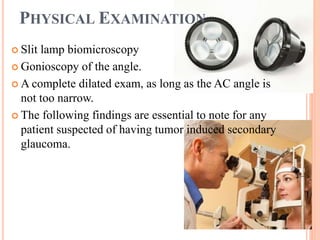
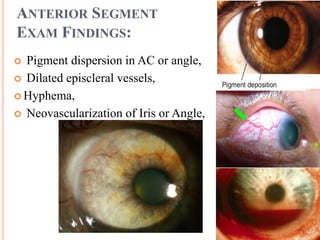
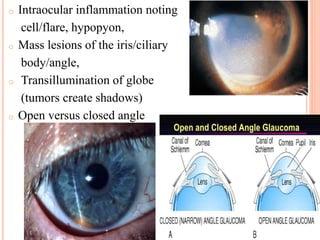
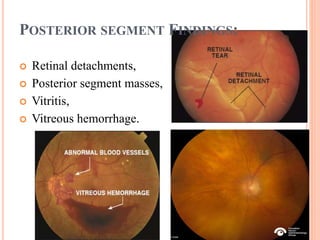
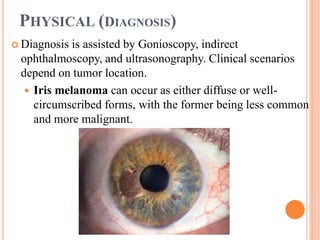
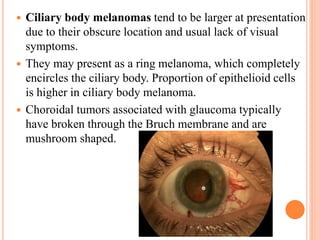
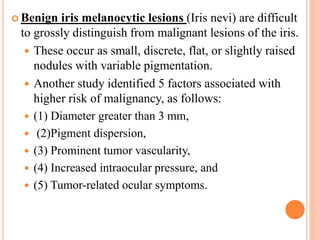
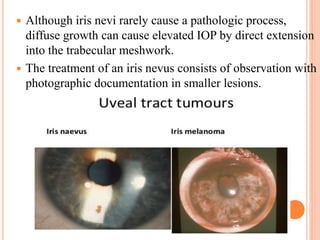
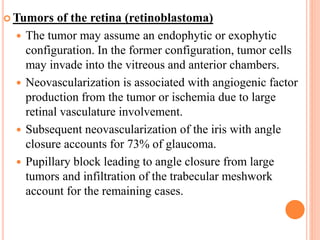
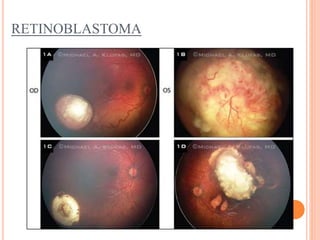
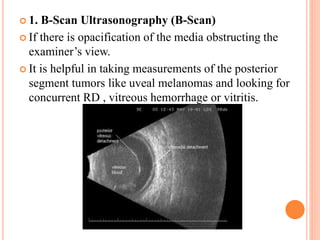
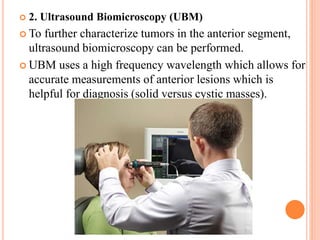
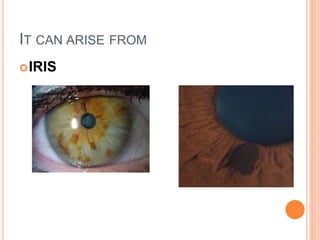
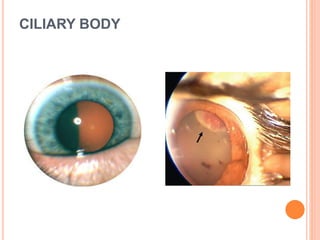
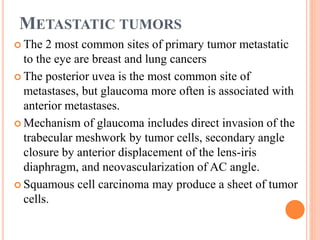
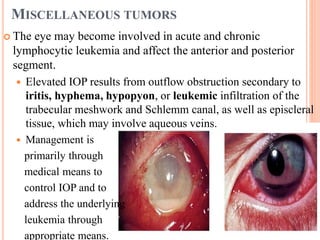
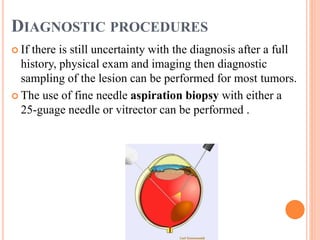
Intraocular tumors can cause secondary glaucoma through several mechanisms. The most common intraocular tumors that cause glaucoma are iris and ciliary body melanomas. These tumors can lead to glaucoma by directly invading the anterior chamber angle, releasing pigment that obstructs the angle, or causing inflammation and neovascularization of the angle. Diagnosis involves a thorough exam including gonioscopy and imaging like ultrasound to identify the location and characteristics of the tumor. The document focuses on the various pathophysiological mechanisms by which different types of intraocular tumors can cause a rise in intraocular pressure and secondary glaucoma.