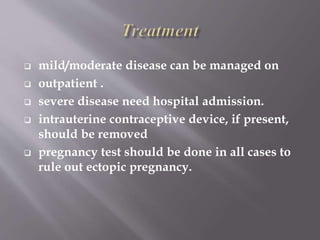
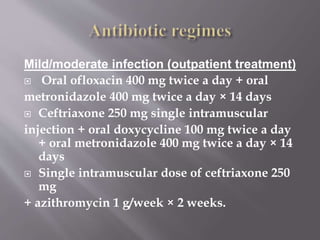
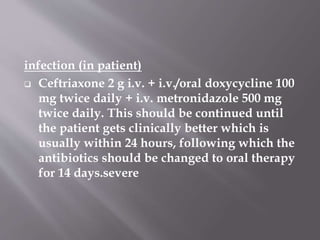
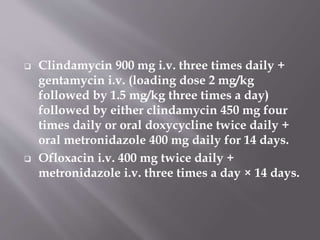
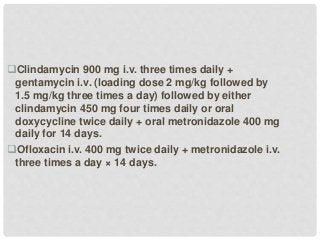
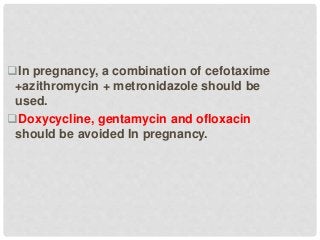
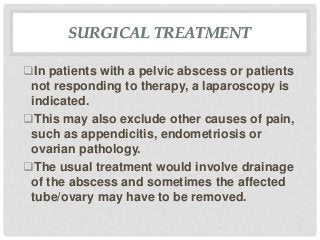
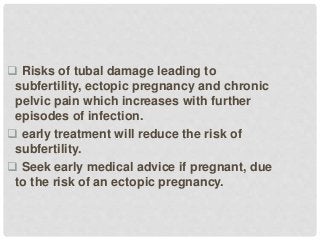
Pelvic inflammatory disease is caused by infections like chlamydia and gonorrhea that spread from the cervix to the fallopian tubes and other female reproductive organs. Left untreated, it can cause tubal scarring and blockages leading to ectopic pregnancy or infertility. Symptoms include abdominal and pelvic pain, abnormal bleeding, and discharge. Treatment involves antibiotics to treat the infection. For severe cases, patients may need to be hospitalized.