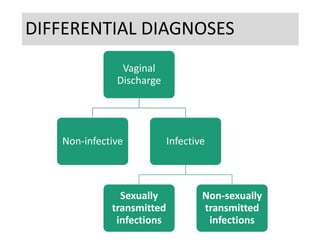
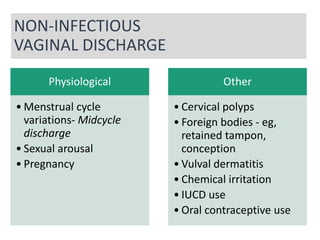
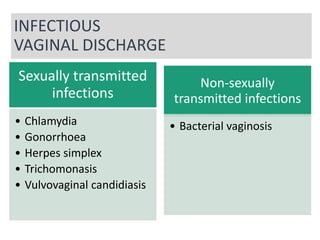
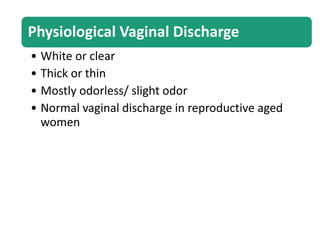
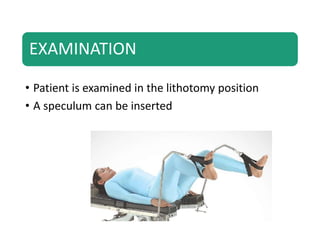
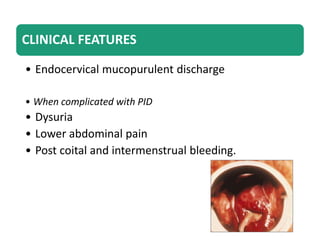
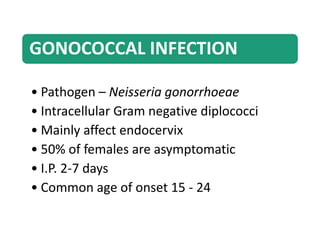
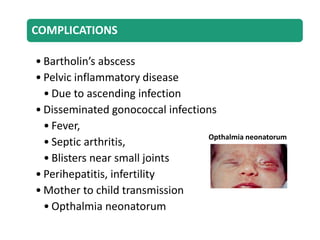
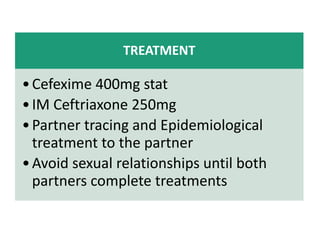
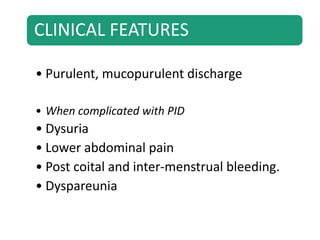
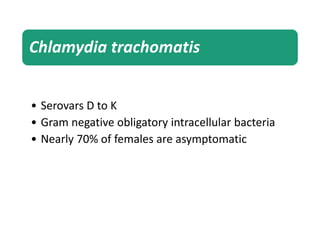
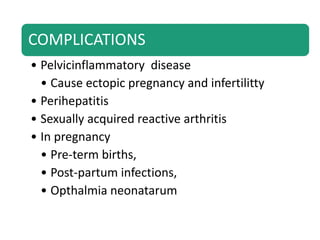
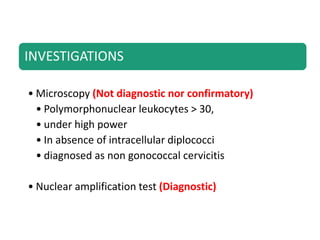
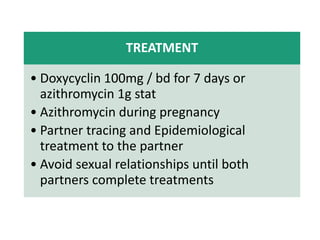
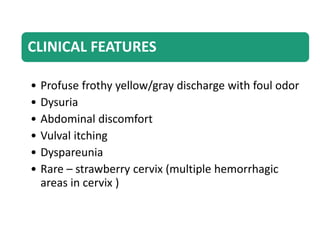
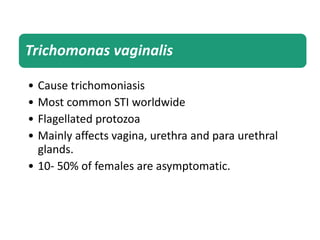
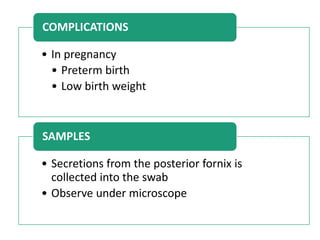
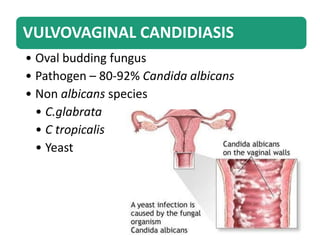
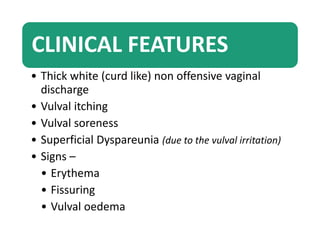
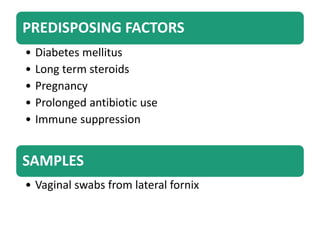
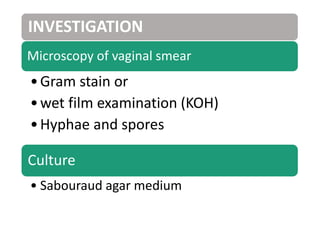
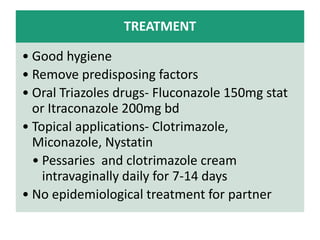
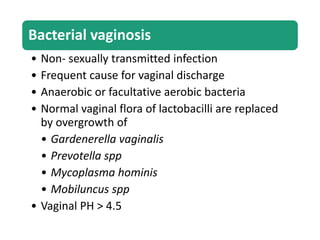
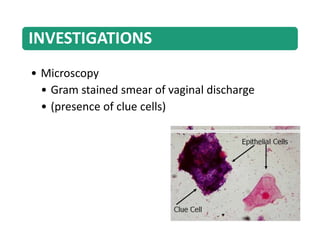
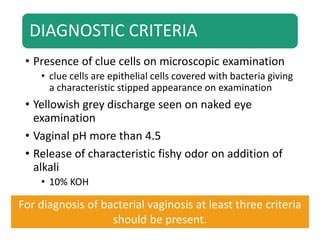
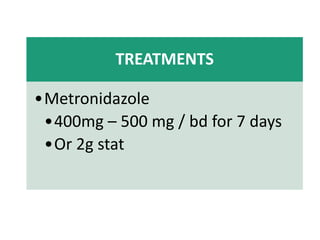
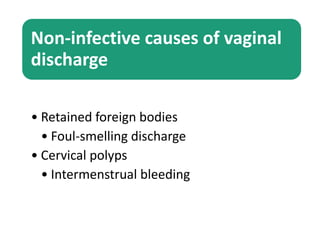
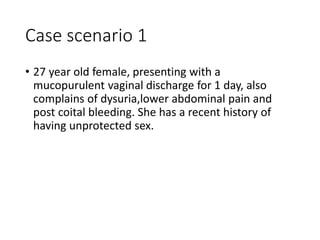
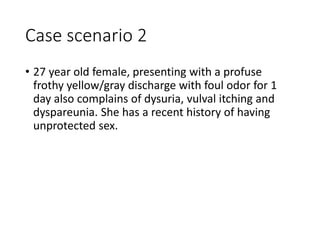
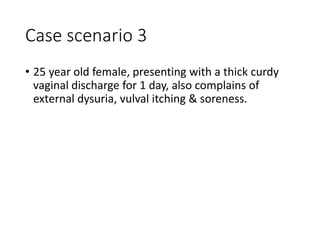
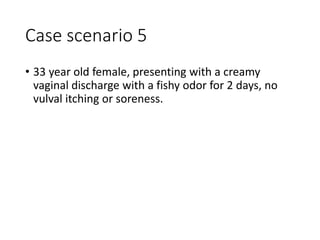
The document provides an overview of vaginal discharge, including its differential diagnoses, history taking strategies, clinical features of various sexually transmitted and non-sexually transmitted infections, and treatment options. It outlines physiological and pathological causes, emphasizing the importance of proper history and examination for accurate diagnosis. Case scenarios are also presented to illustrate common clinical presentations in women visiting STI clinics.