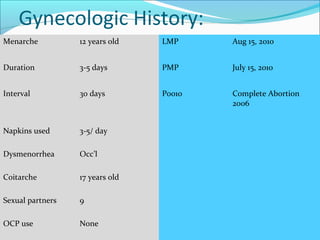
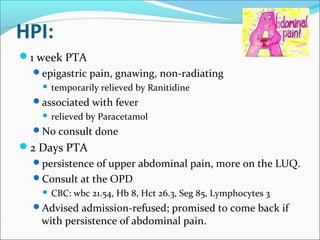
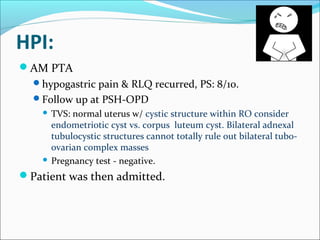
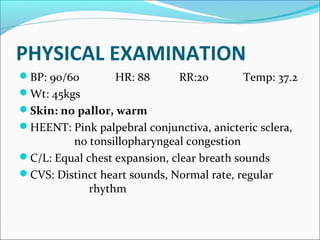
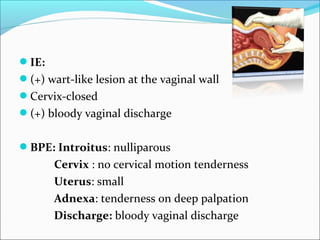
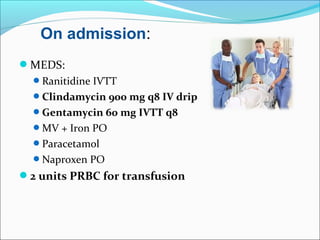
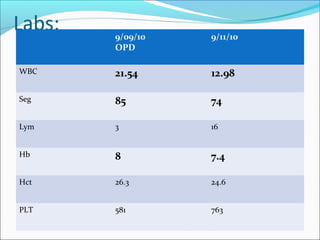
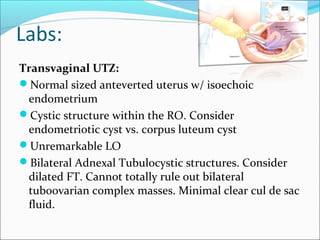
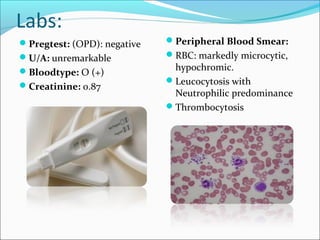
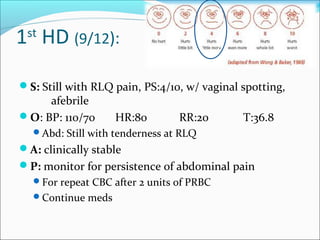
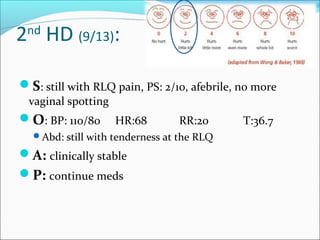
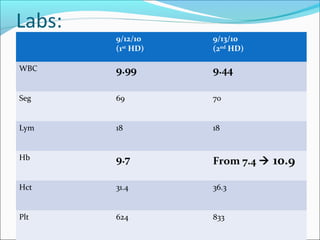
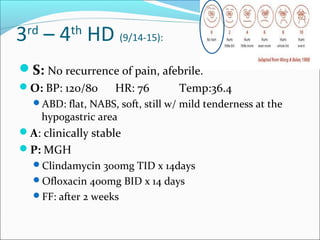
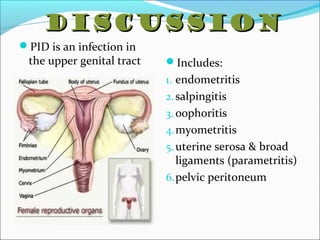
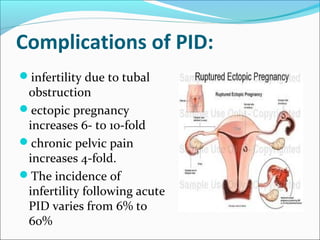
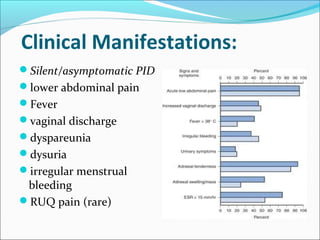
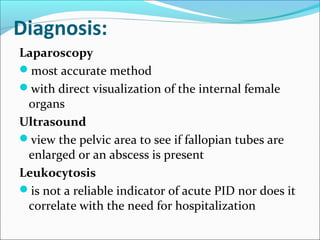
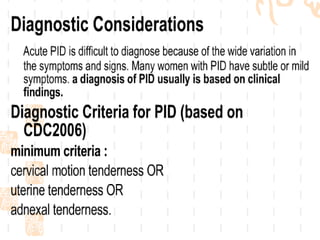
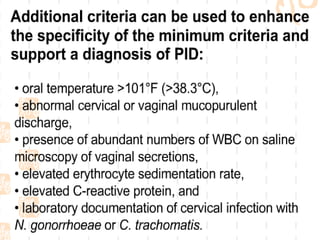
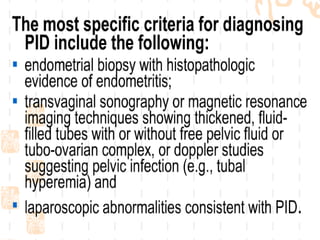
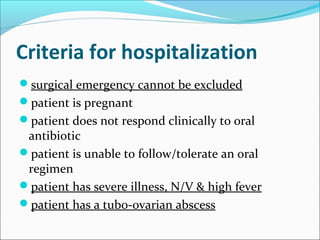
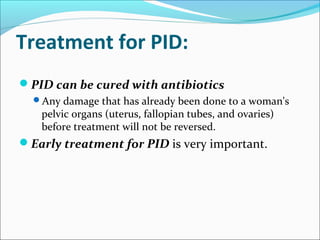
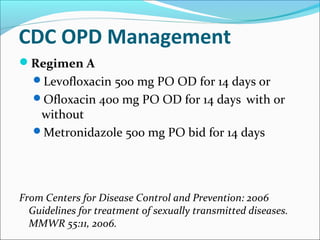
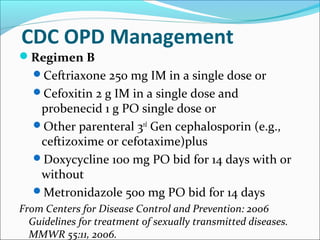
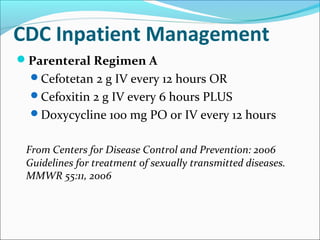
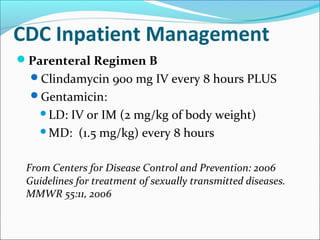
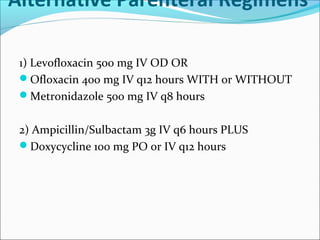
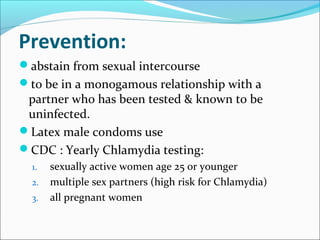
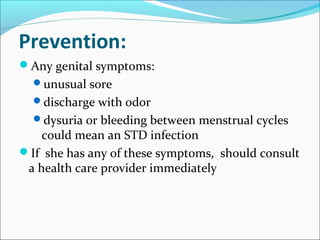
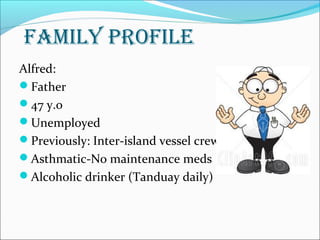
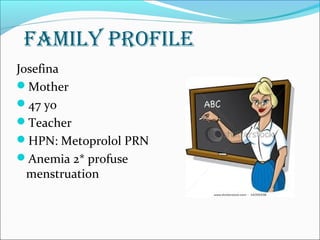
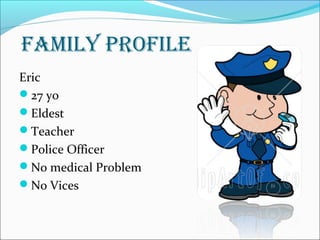
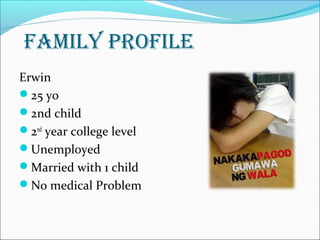
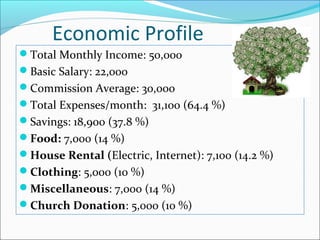
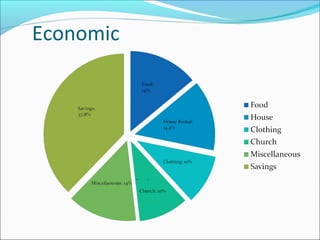
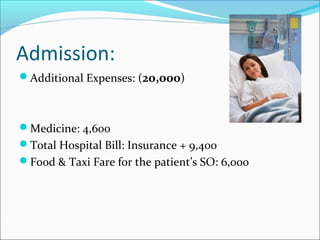
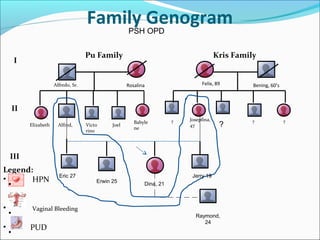
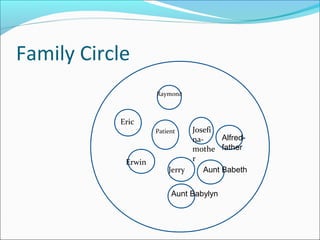
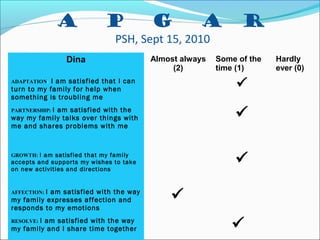
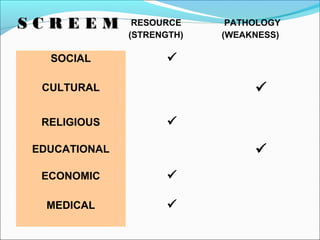
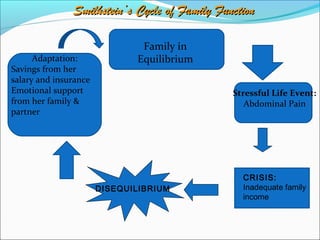
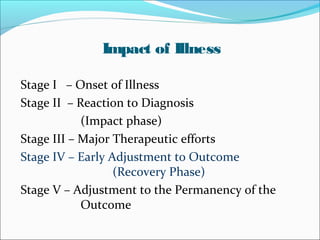
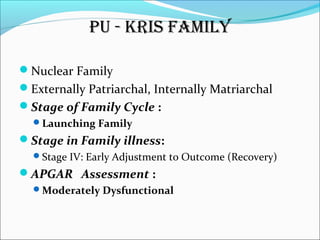
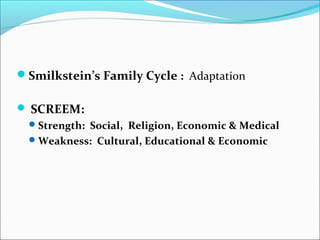
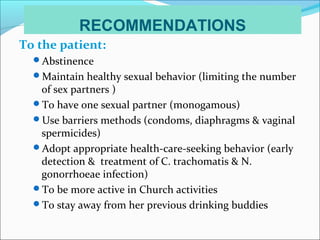
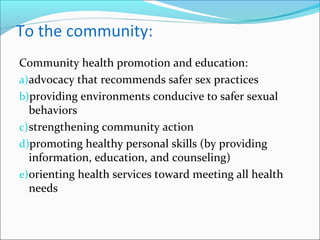
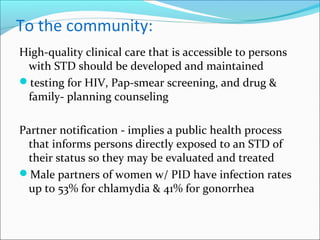
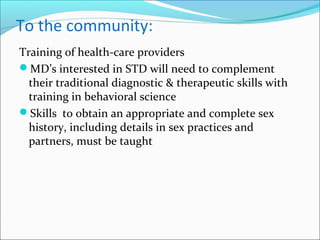
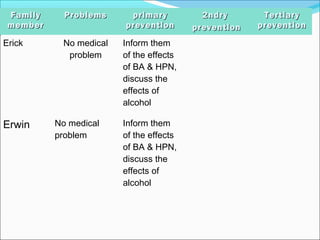
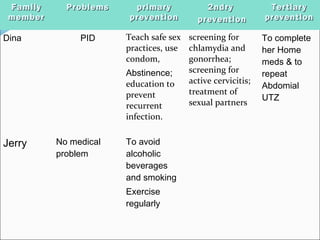
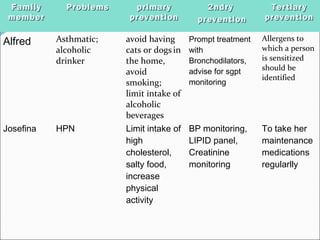
This document presents the case of a 21-year-old female admitted for abdominal pain. She has a history of smoking and is diagnosed with pelvic inflammatory disease (PID) based on symptoms of abdominal pain and vaginal discharge. She is treated with antibiotics and blood transfusions and shows improvement. The document also discusses PID, its causes, symptoms, diagnosis and treatment guidelines. It profiles the patient's family and their economic situation.