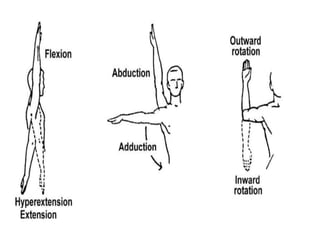
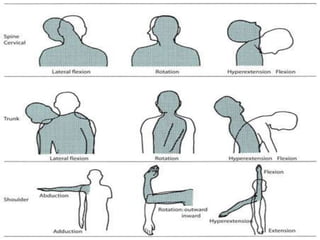
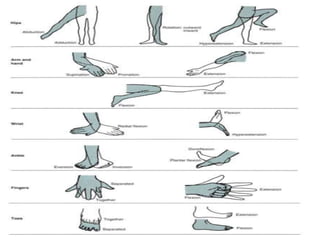
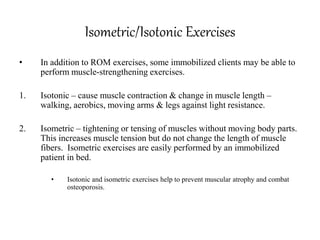
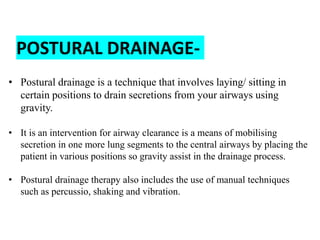
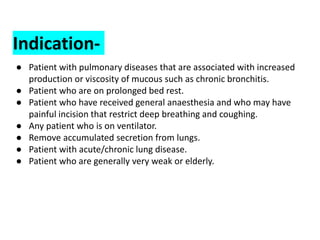
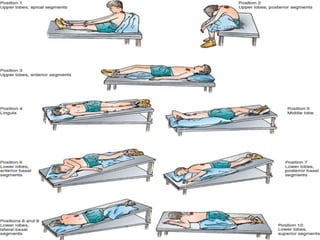
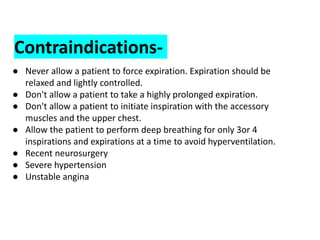
The document discusses mobility, range of motion exercises, and postural drainage techniques. It defines mobility and immobility as endpoints on a continuum, with many degrees of partial immobility in between. It describes active, passive and active assisted range of motion exercises and their purposes in maintaining joint function and flexibility. It provides details on different postural drainage positions and manual techniques like percussion, vibration and shaking used to drain secretions from the lungs into larger airways.