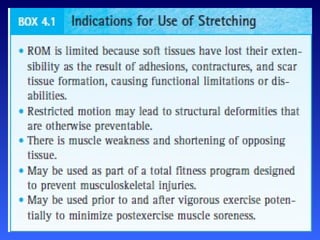
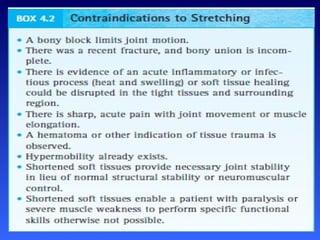
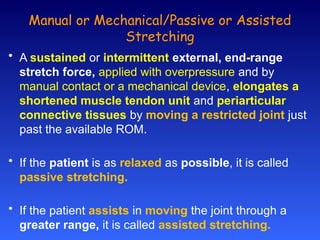
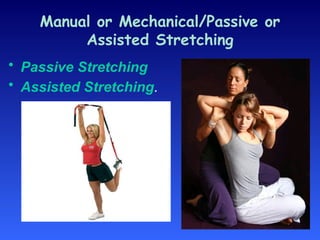
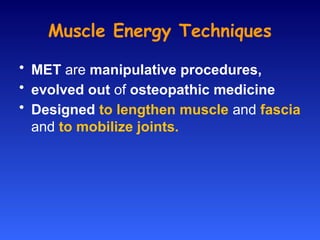
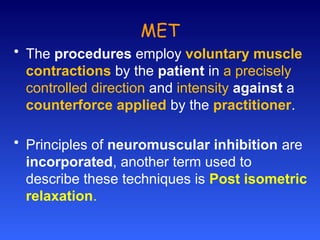
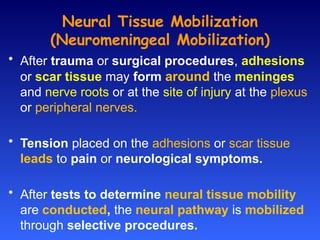
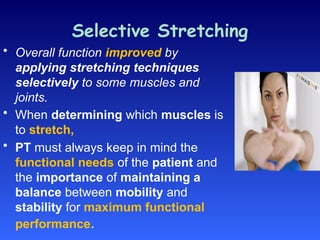
The document outlines various therapeutic interventions designed to enhance soft tissue mobility and flexibility, including manual stretching techniques, self-stretching, and neuromuscular facilitation. It discusses the importance of determining appropriate stretching methods based on patient needs and circumstances, including potential risks of overstretching and joint instability. Overall, the document emphasizes a balanced approach to stretching that conserves mobility while maintaining stability for optimal functional performance.