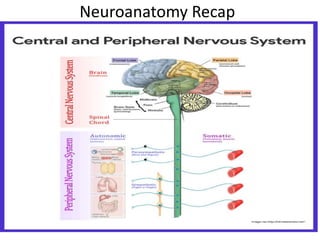
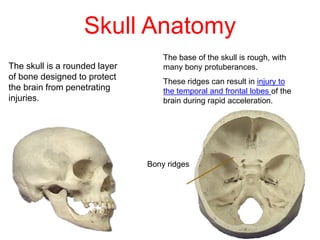
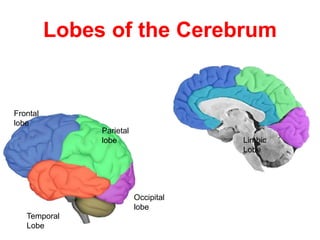
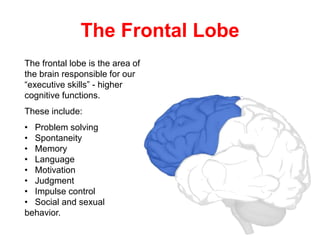
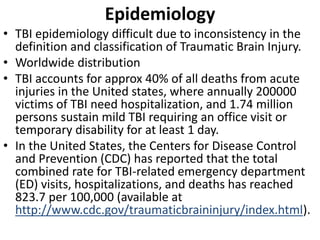
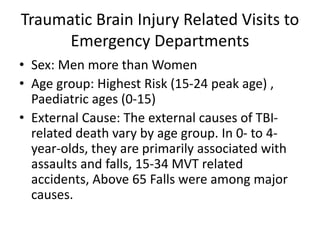
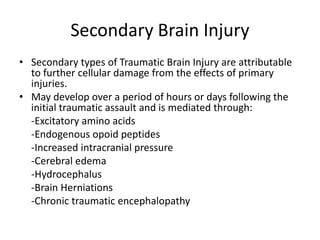
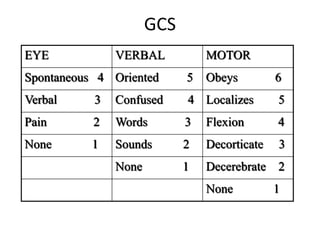
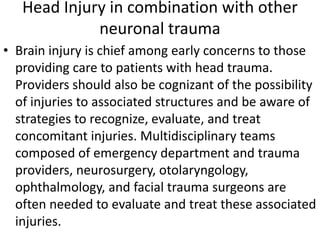
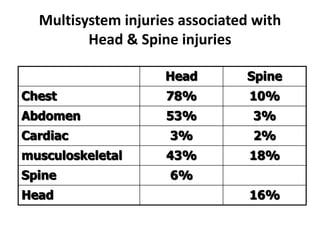
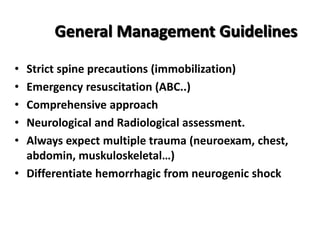
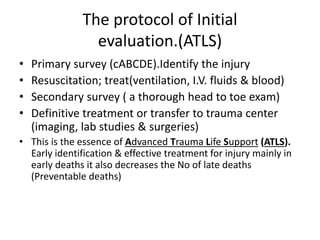
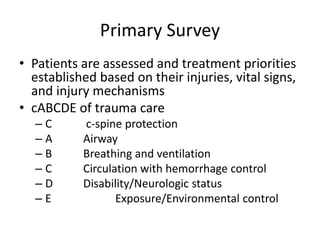
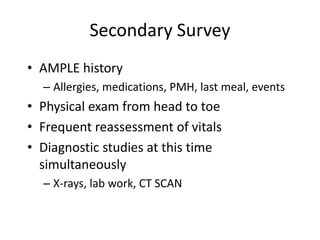
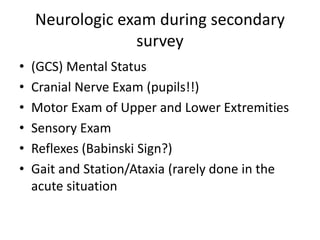
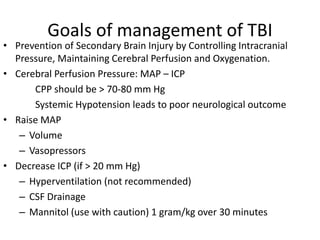
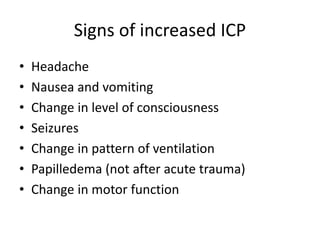
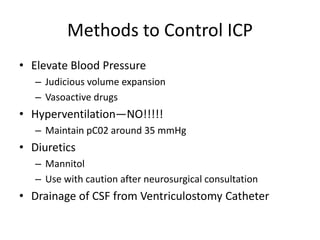
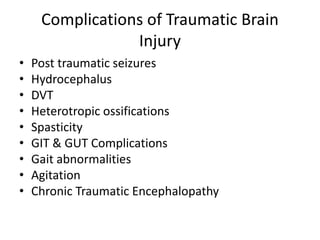
This document provides an overview of traumatic brain injury (TBI) and associated neurotrauma. It defines TBI and discusses the pathophysiology, including primary and secondary injury mechanisms. It also covers epidemiology, risk factors, assessment tools like the Glasgow Coma Scale, and management principles like the ATLS protocol. Key goals in TBI management are preventing secondary brain injury by controlling intracranial pressure and maintaining cerebral blood flow and oxygenation. The document additionally addresses spinal cord injuries, multisystem trauma patterns, and potential TBI complications.