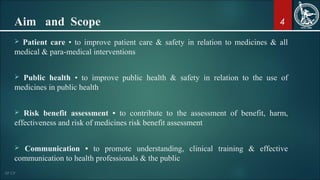
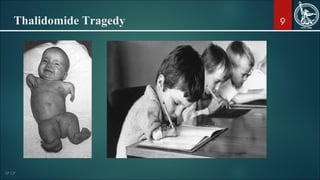
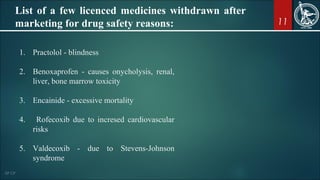
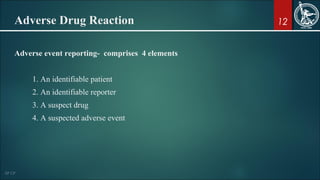
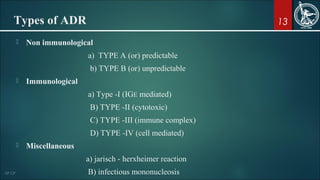
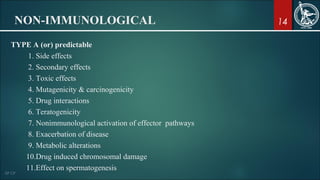
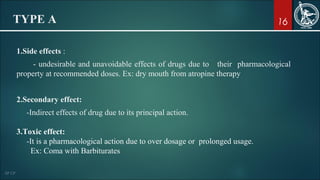
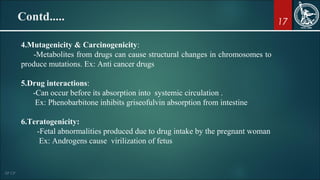
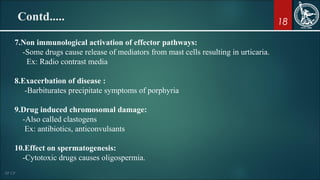
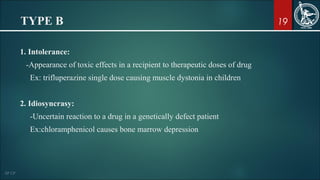
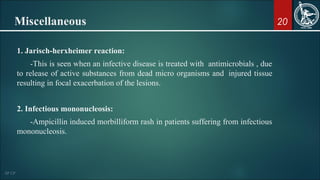
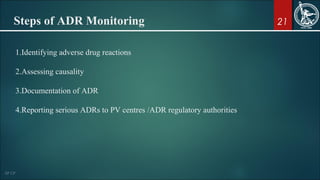
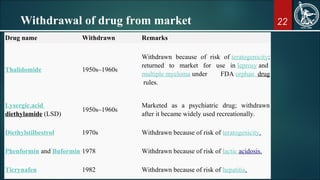
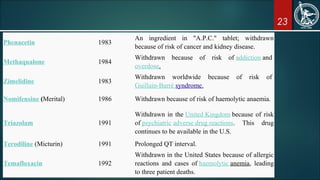
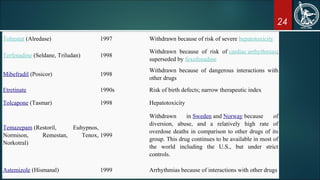
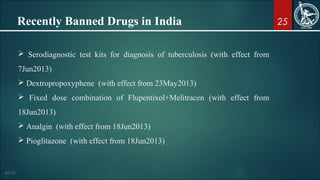
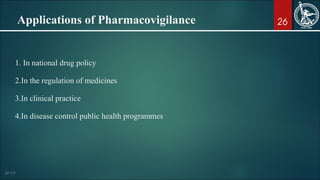
The document provides a comprehensive overview of pharmacovigilance, which involves the monitoring and prevention of adverse drug reactions (ADRs) in pharmaceutical products. It highlights the importance of pharmacovigilance in improving patient care, ensuring public health safety, and the ethical necessity of reporting serious drug reactions. Additionally, it discusses historical drug disasters that led to the establishment of regulatory mechanisms and outlines the types of ADRs, steps for monitoring them, and gives examples of drugs that have been withdrawn due to safety concerns.