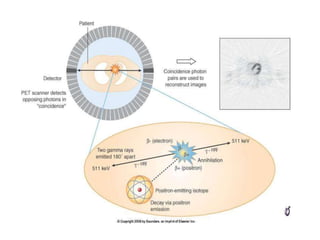
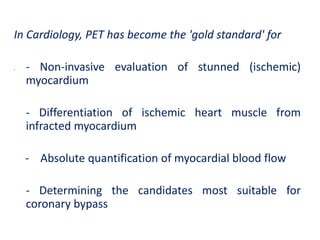
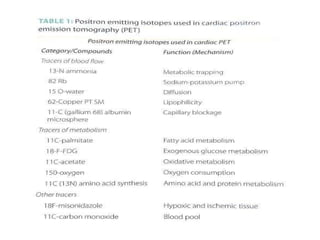
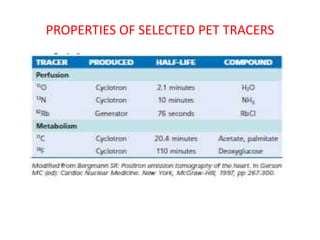
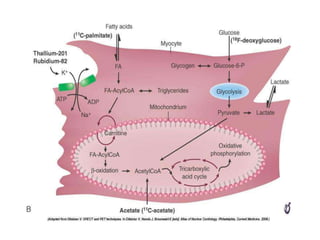
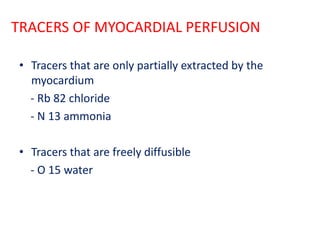
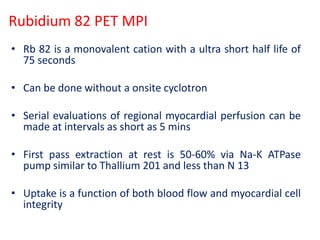
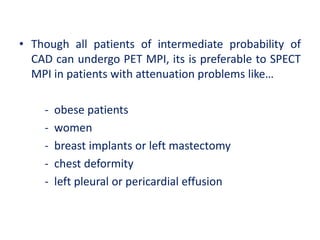
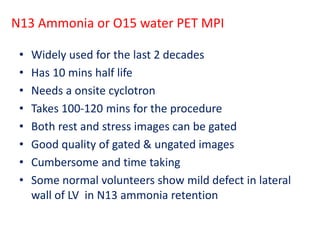
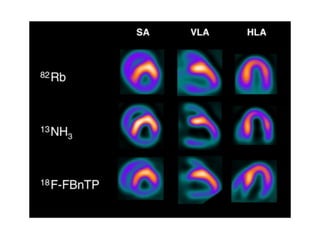
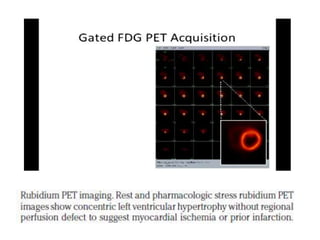
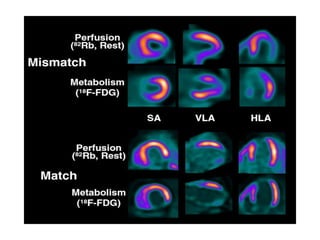
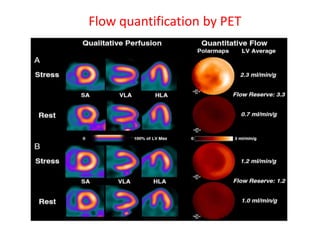
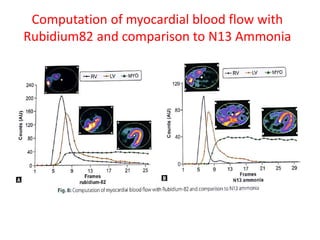
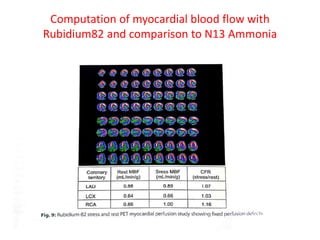
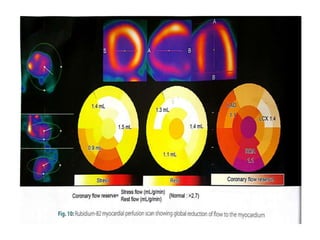
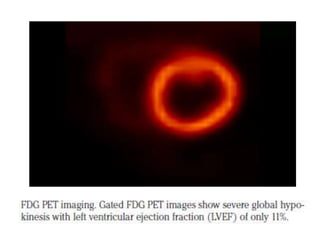
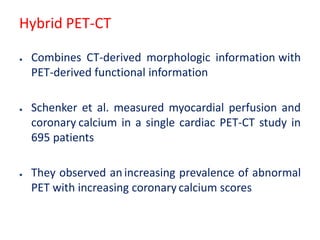
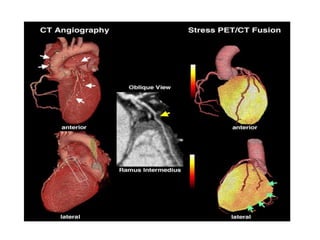
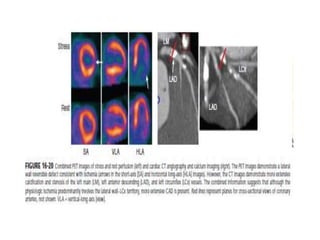
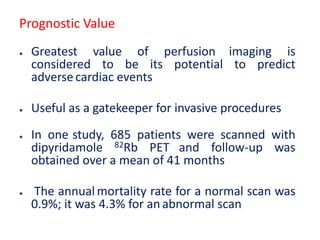
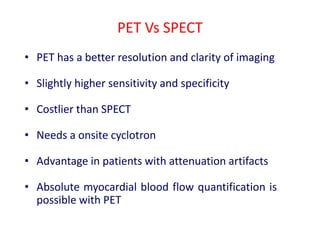
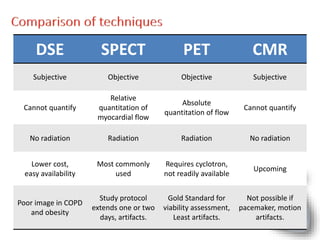
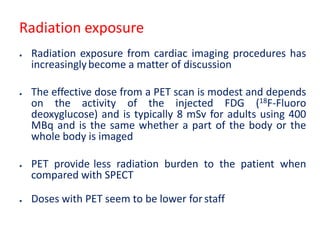
PET imaging provides functional information about metabolic processes in the body. It is used in cardiology to non-invasively evaluate myocardial blood flow, metabolism, and viability. Tracers such as rubidium-82, ammonia-13, fluorodeoxyglucose, and oxygen-15 are injected and imaged to assess perfusion and glucose uptake, identifying ischemic, hibernating, and infarcted tissue. PET MPI has high sensitivity and specificity for CAD detection compared to other tests.