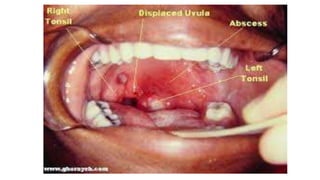
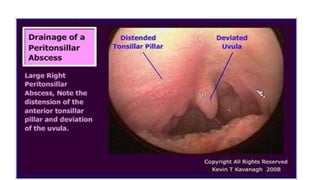
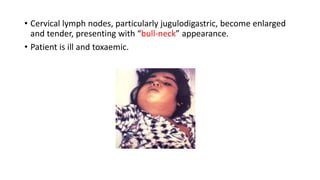
Peritonsillar abscess, often following acute tonsillitis, is a collection of pus in the peritonsillar space causing symptoms like throat pain, fever, and trismus. Diagnosis involves physical examination and imaging, while management includes intravenous antibiotics, analgesics, and possible incision and drainage. Complications may arise, including airway obstruction and septicemia, necessitating close monitoring and possible surgical intervention.