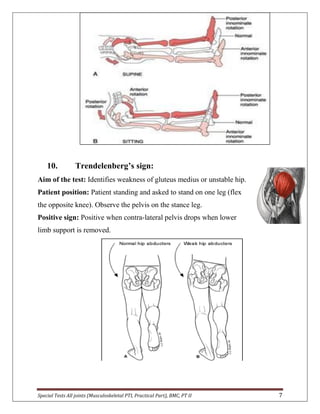
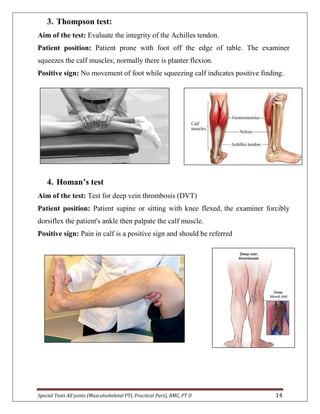
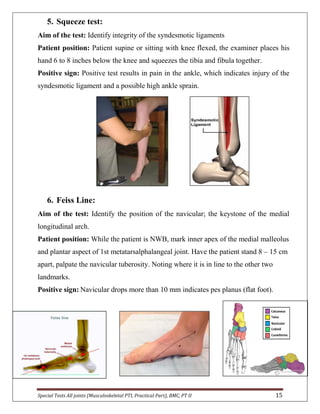
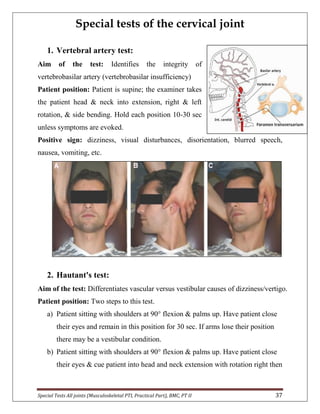
The document provides descriptions of special tests for various musculoskeletal joints including the hip, knee, ankle, foot, lumbar spine, shoulder, elbow, wrist, hand, and cervical spine. For each joint, 2-10 special tests are described, including the aim of the test, patient positioning, and what constitutes a positive finding. The special tests are used to identify tightness, laxity, nerve irritation, and other dysfunctions of the joints and surrounding tissues.