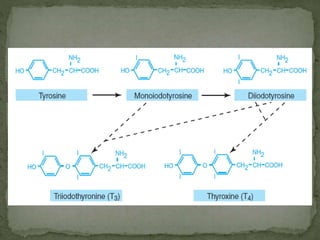
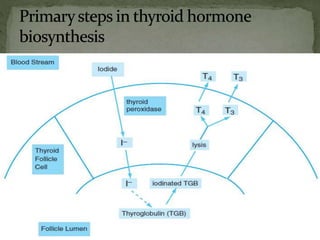
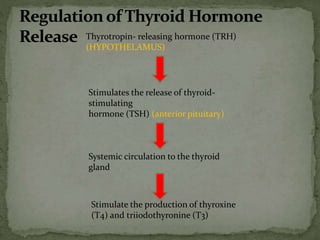
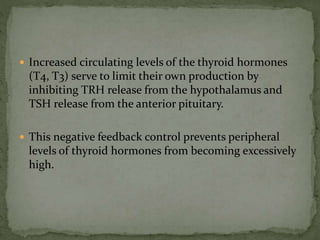
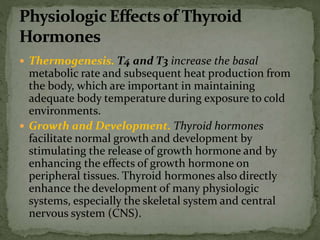
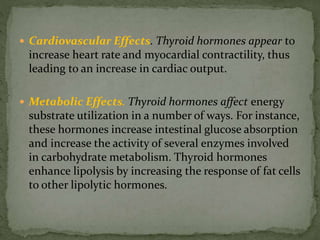
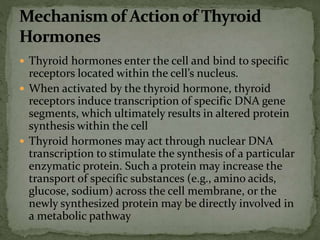
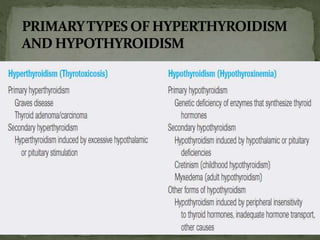
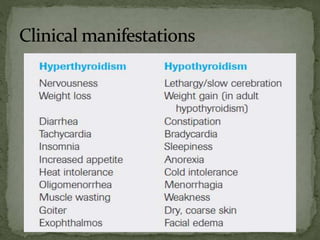
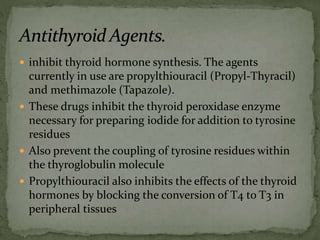
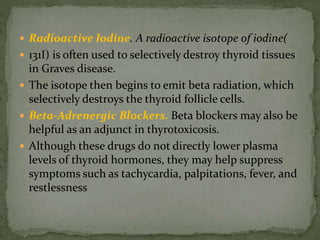
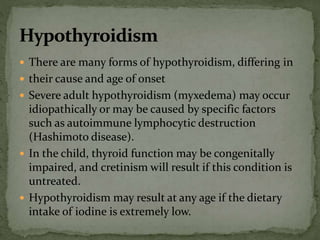
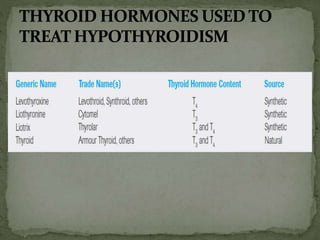
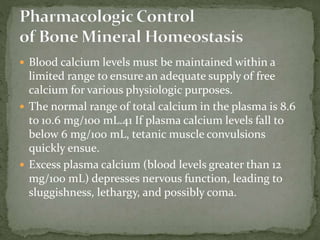
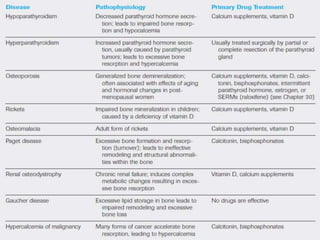
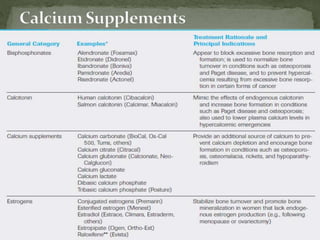
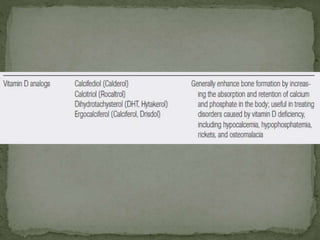
The document discusses the endocrine functions of the thyroid gland, parathyroid glands, and their roles in calcium and bone homeostasis. Specifically, it describes how thyroid hormones are synthesized and regulated, their effects on growth, metabolism and other body systems. It also explains how parathyroid hormone regulates blood calcium levels by acting on bone, kidneys and intestines. The importance of maintaining normal calcium levels and balancing bone formation and resorption is emphasized.