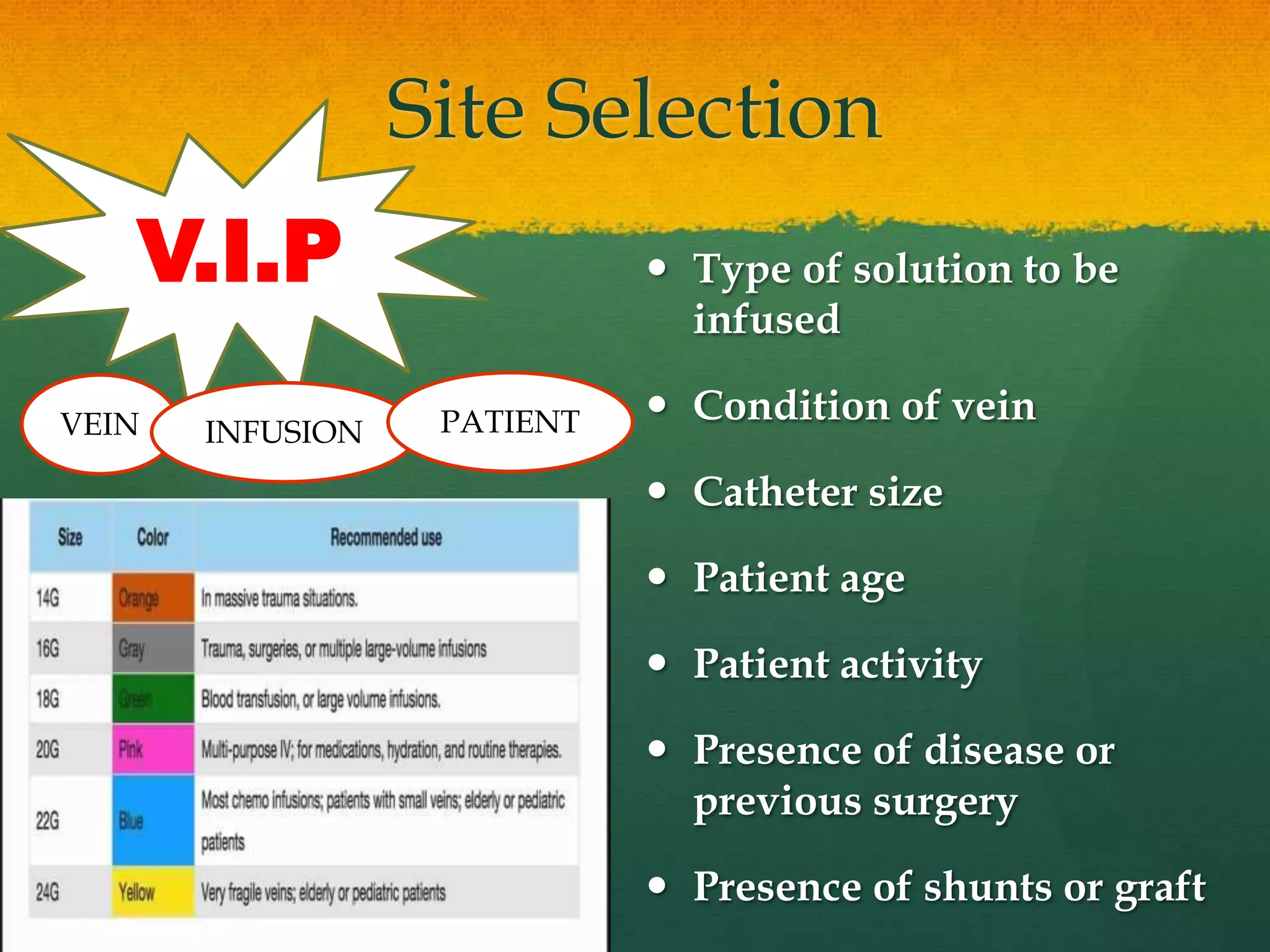
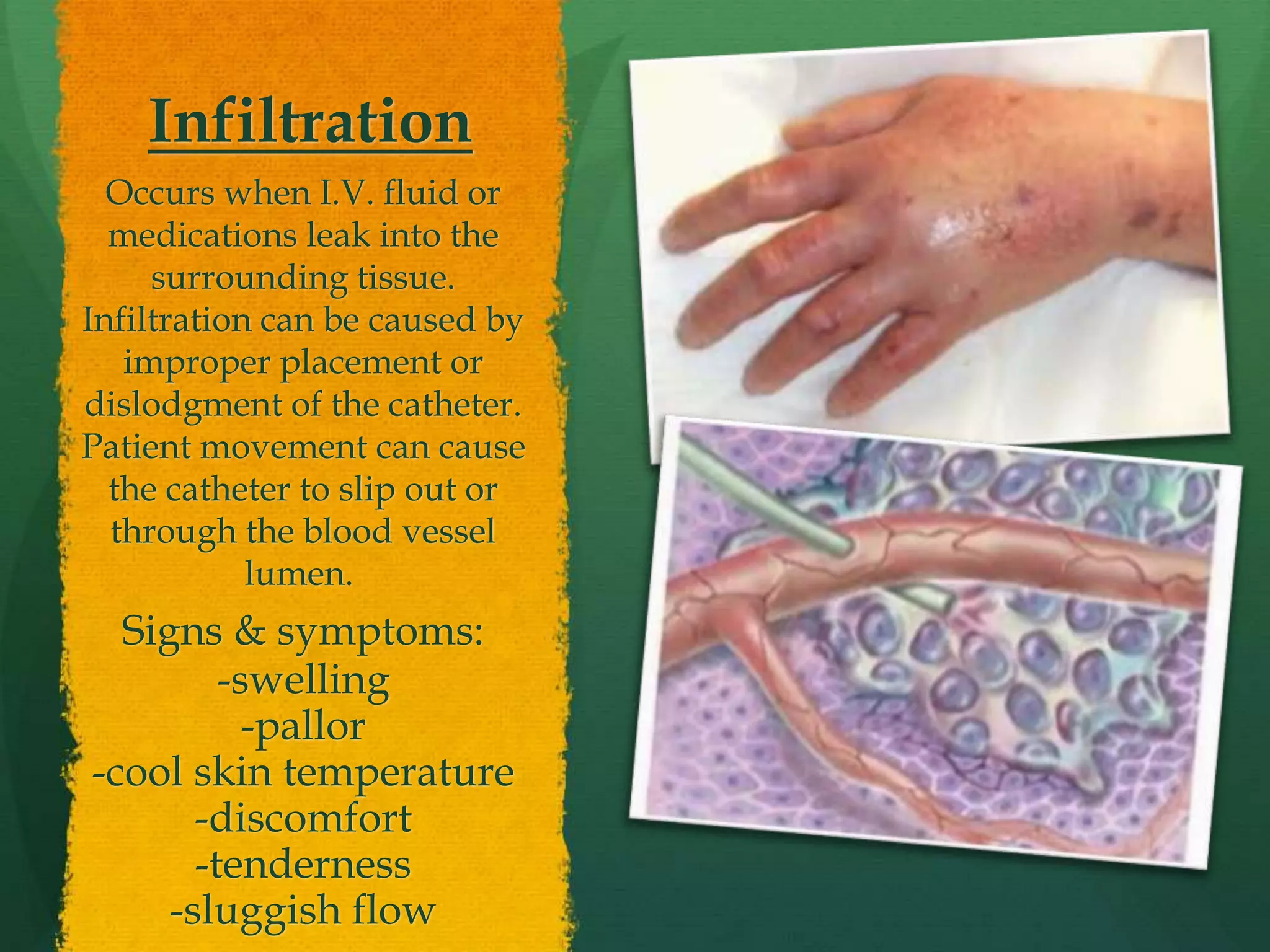
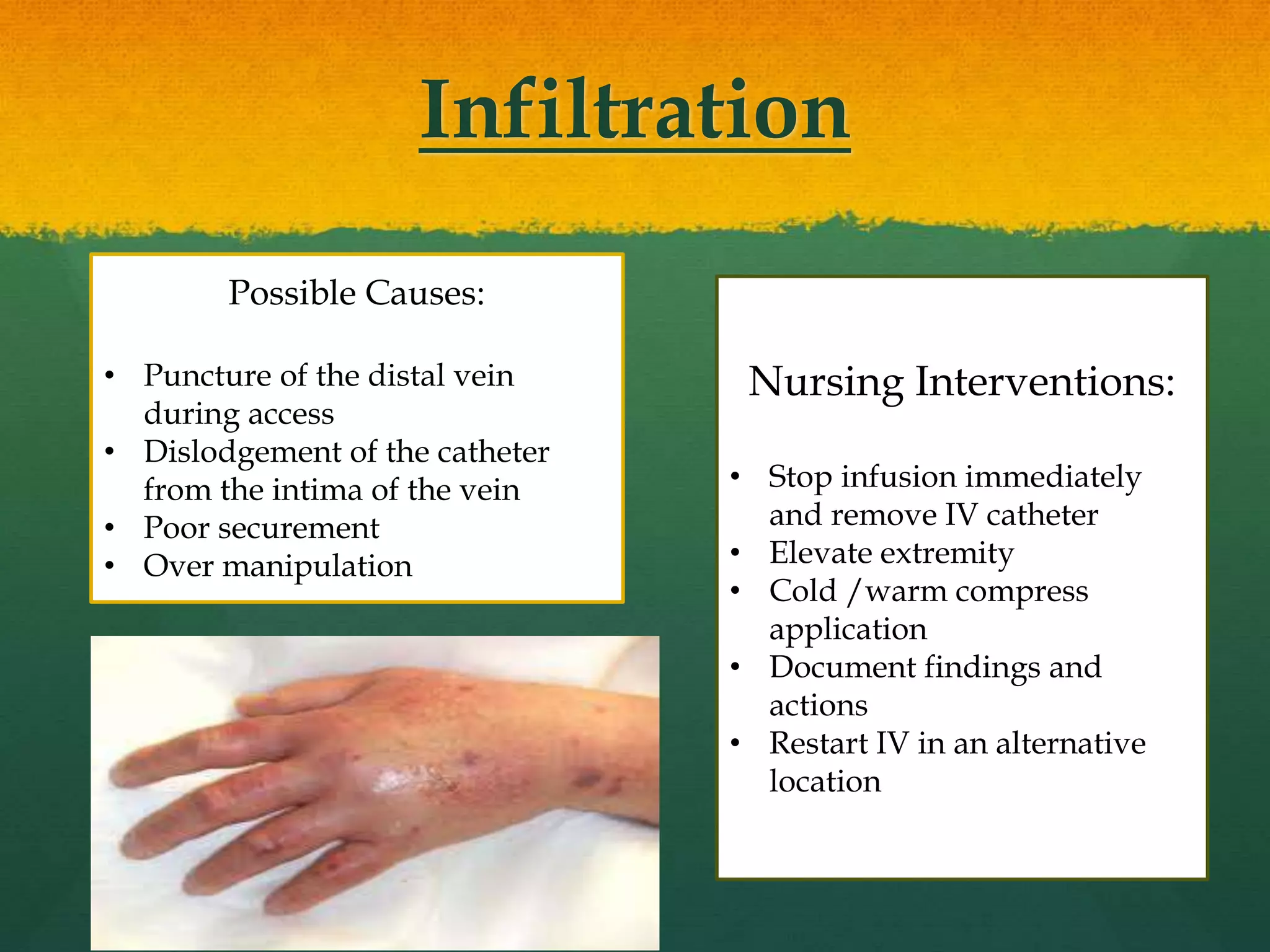
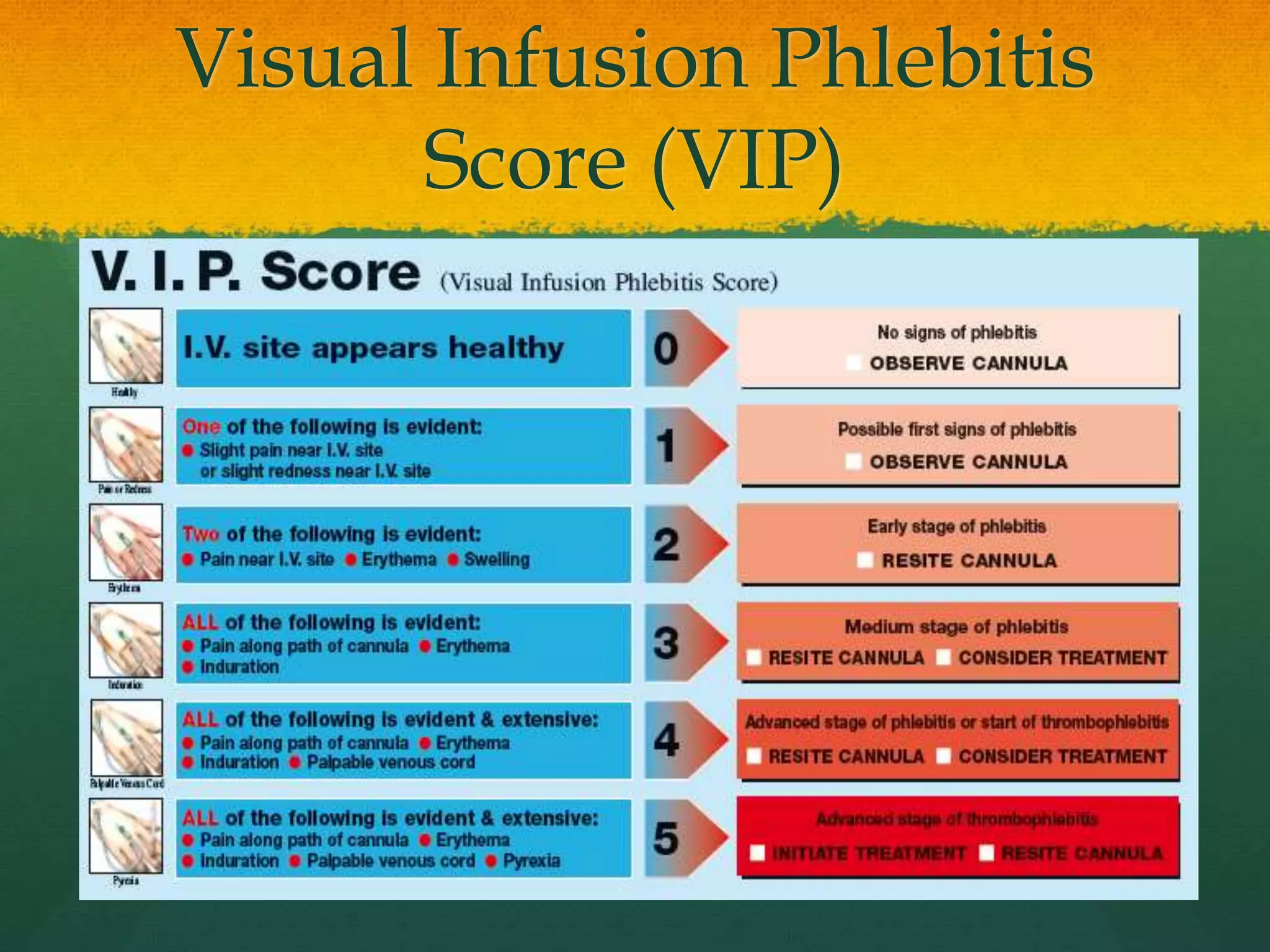
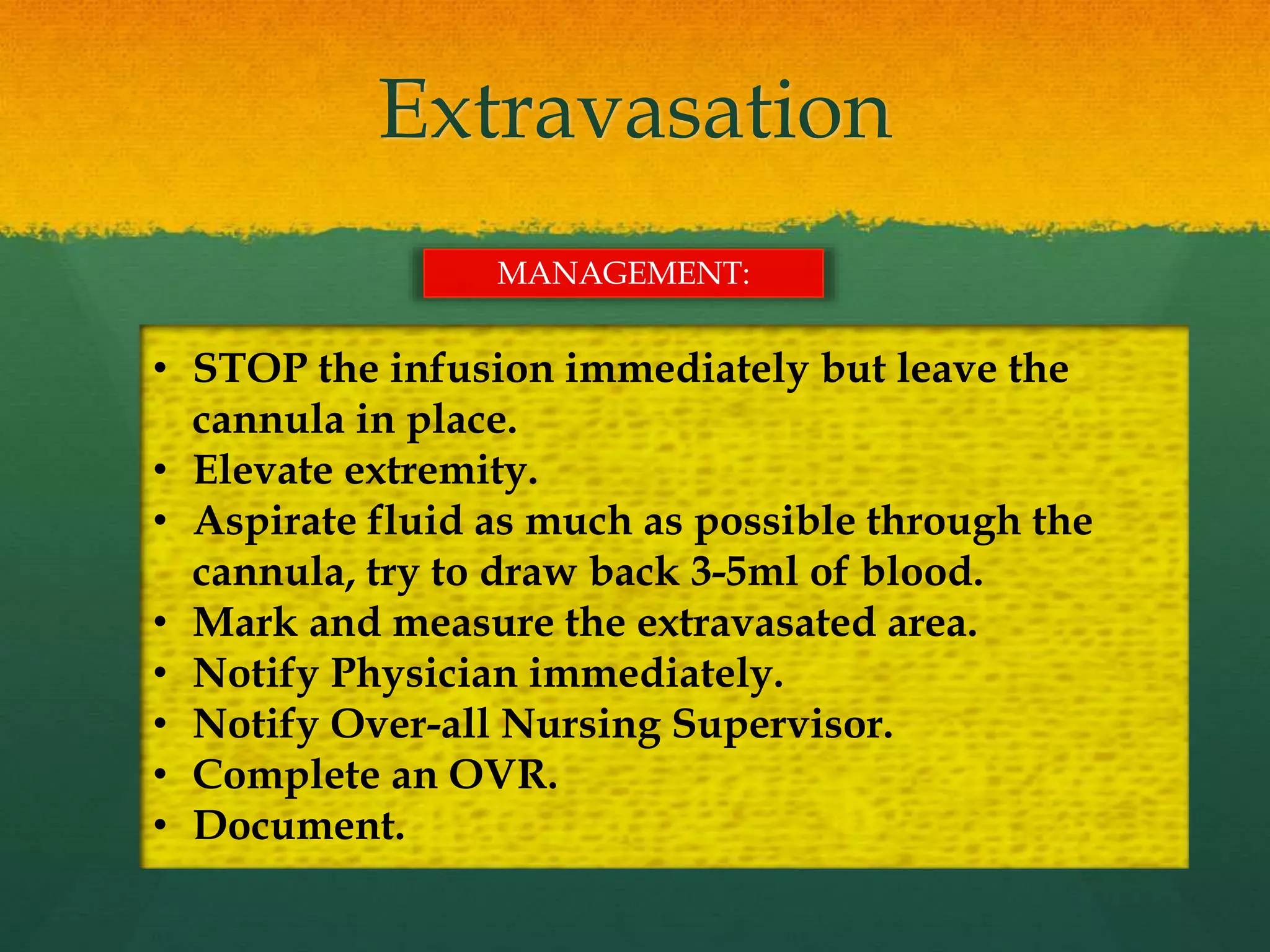
This document discusses IV therapy indications and complications. It begins by noting that over 85% of hospitalized patients receive IV therapy. Common complications include infiltration where fluid leaks into tissue, phlebitis which is vein inflammation, hematoma involving blood leakage, extravasation where vesicants leak out of veins, and air embolism or fluid overload. The document provides details on signs and symptoms and management of each complication to help nurses properly assess, treat and document any issues. It emphasizes the importance of monitoring for early intervention to prevent potential systemic complications.