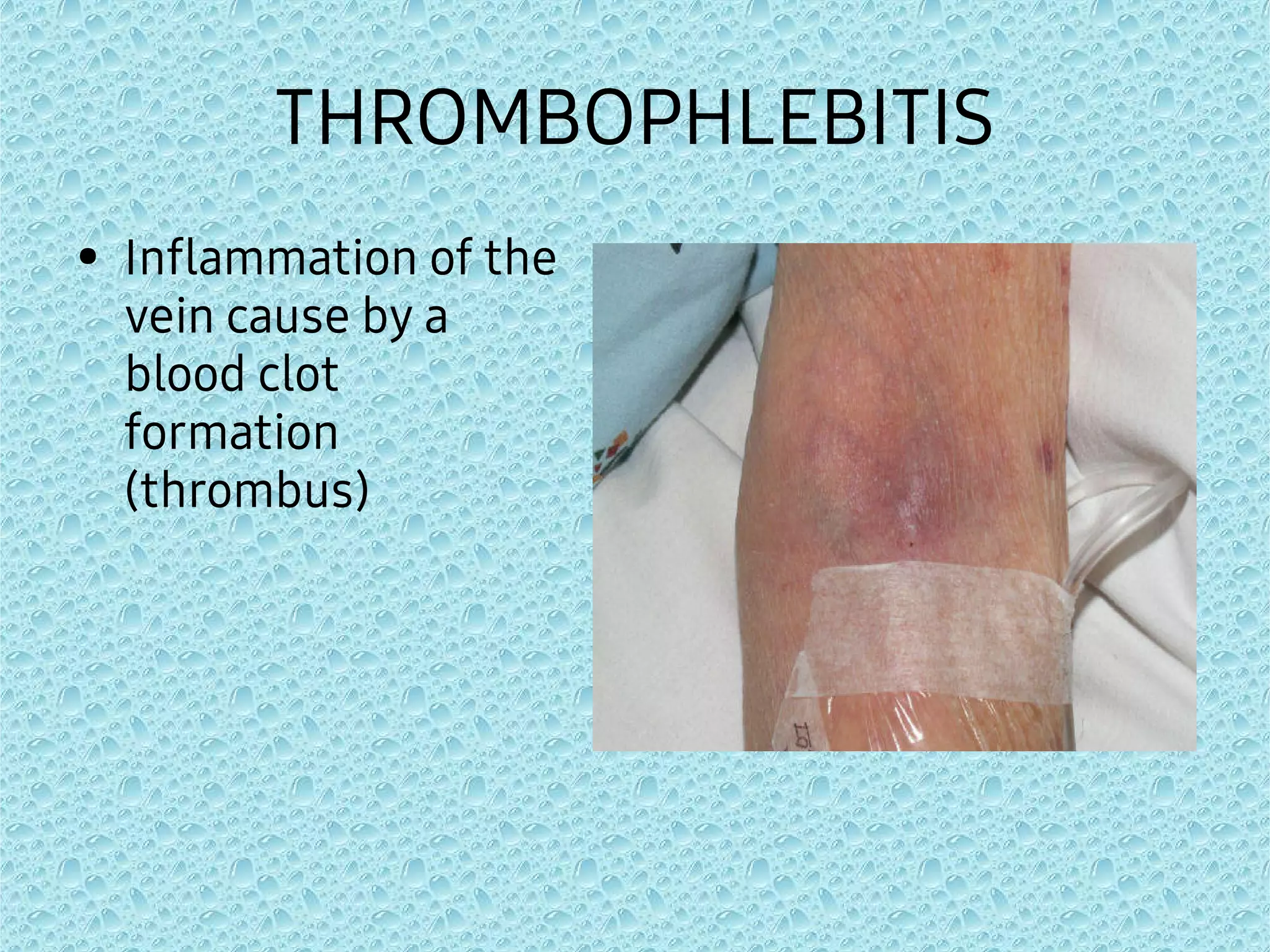
This document discusses various complications that can arise from intravenous (IV) therapy and their prevention and treatment. It covers complications like needlestick injury, phlebitis, infiltration, extravasation, infection, air embolism, and occlusion. For each complication, the summary provides the causes, signs and symptoms, nursing interventions, and preventive measures. The overall goal is to educate on safely managing IV therapy and preventing associated risks.