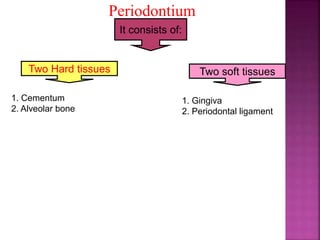
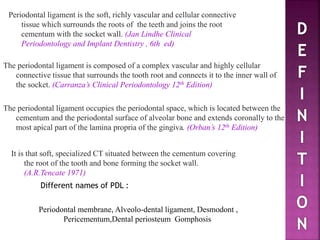
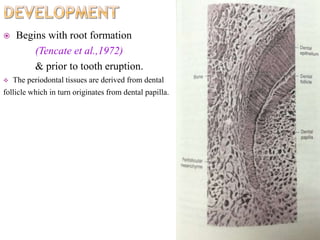
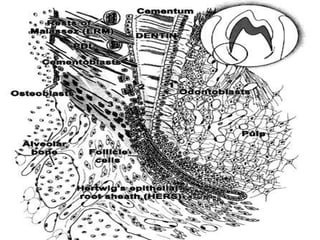
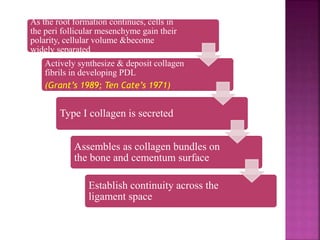
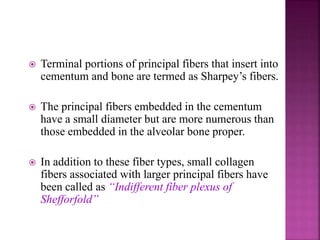
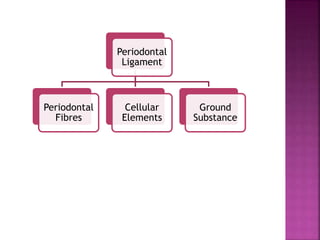
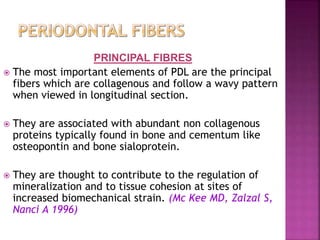
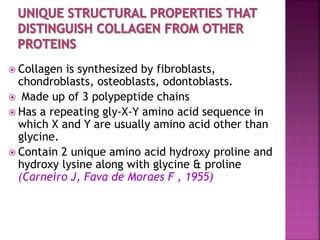
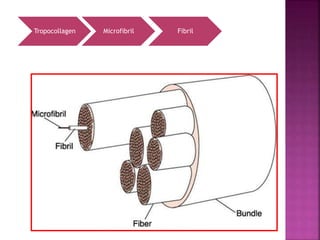
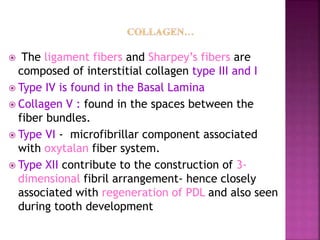
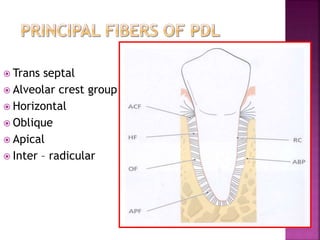
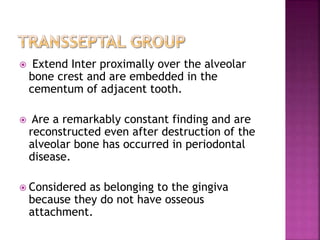
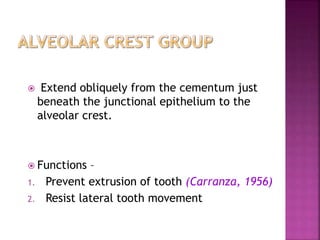
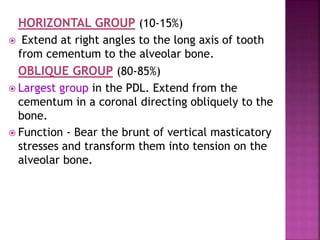
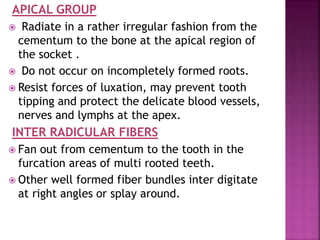
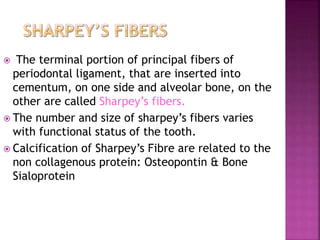
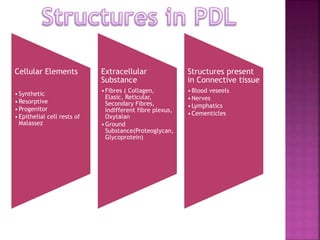
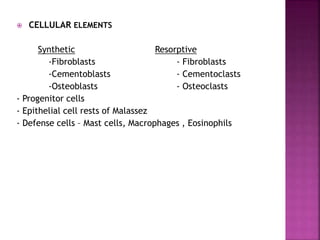
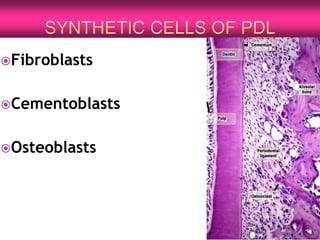
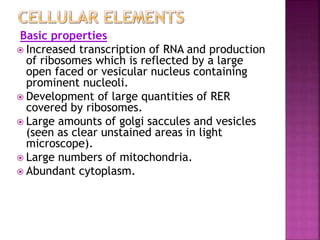
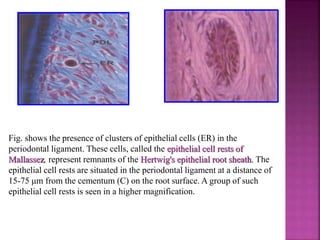
The periodontium is the connective tissue that surrounds and supports the teeth. It consists of gingiva, periodontal ligament, cementum, and alveolar bone. The periodontal ligament is a soft, vascular connective tissue that joins the cementum and alveolar bone. It contains collagen fibers that provide support and flexibility to the teeth. The ligament is populated by fibroblasts that synthesize collagen fibers, as well as other cells like cementoblasts and osteoblasts that maintain the hard tissues.