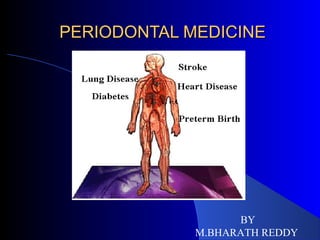
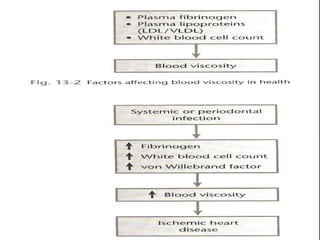
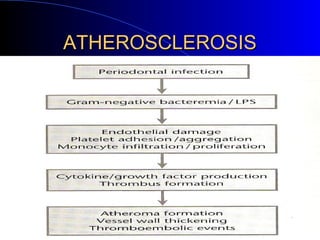
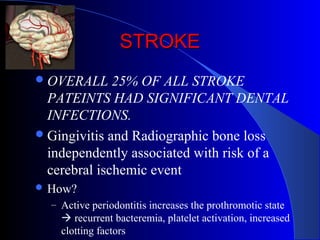
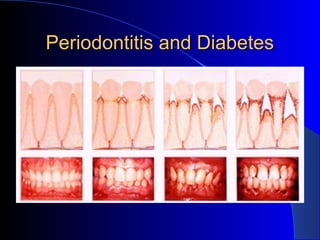
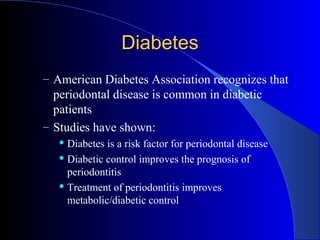
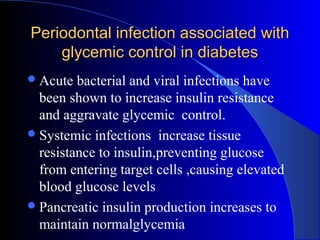
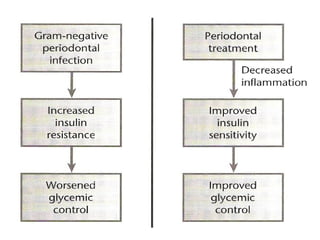
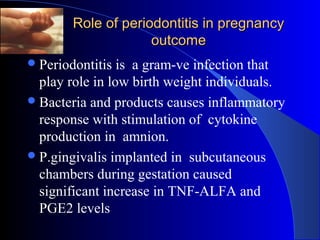
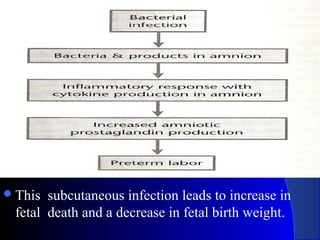
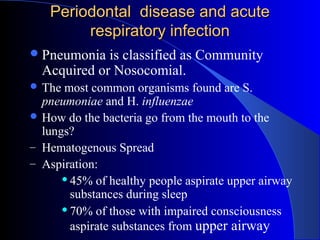
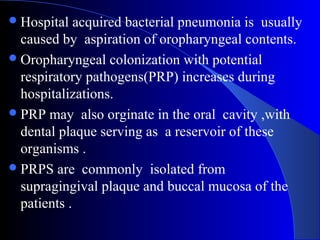
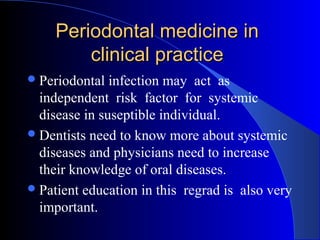
This document discusses the relationship between periodontal disease and various systemic conditions. It begins by providing historical context on how the link between oral and systemic health has been understood over time. Key points discussed include: the era of focal infection theory in the 18th-19th centuries; associations found between periodontitis and coronary heart disease/atherosclerosis, diabetes, pregnancy outcomes, COPD, and acute respiratory infections; and how periodontal medicine knowledge can be applied in clinical practice through interprofessional collaboration and patient education.