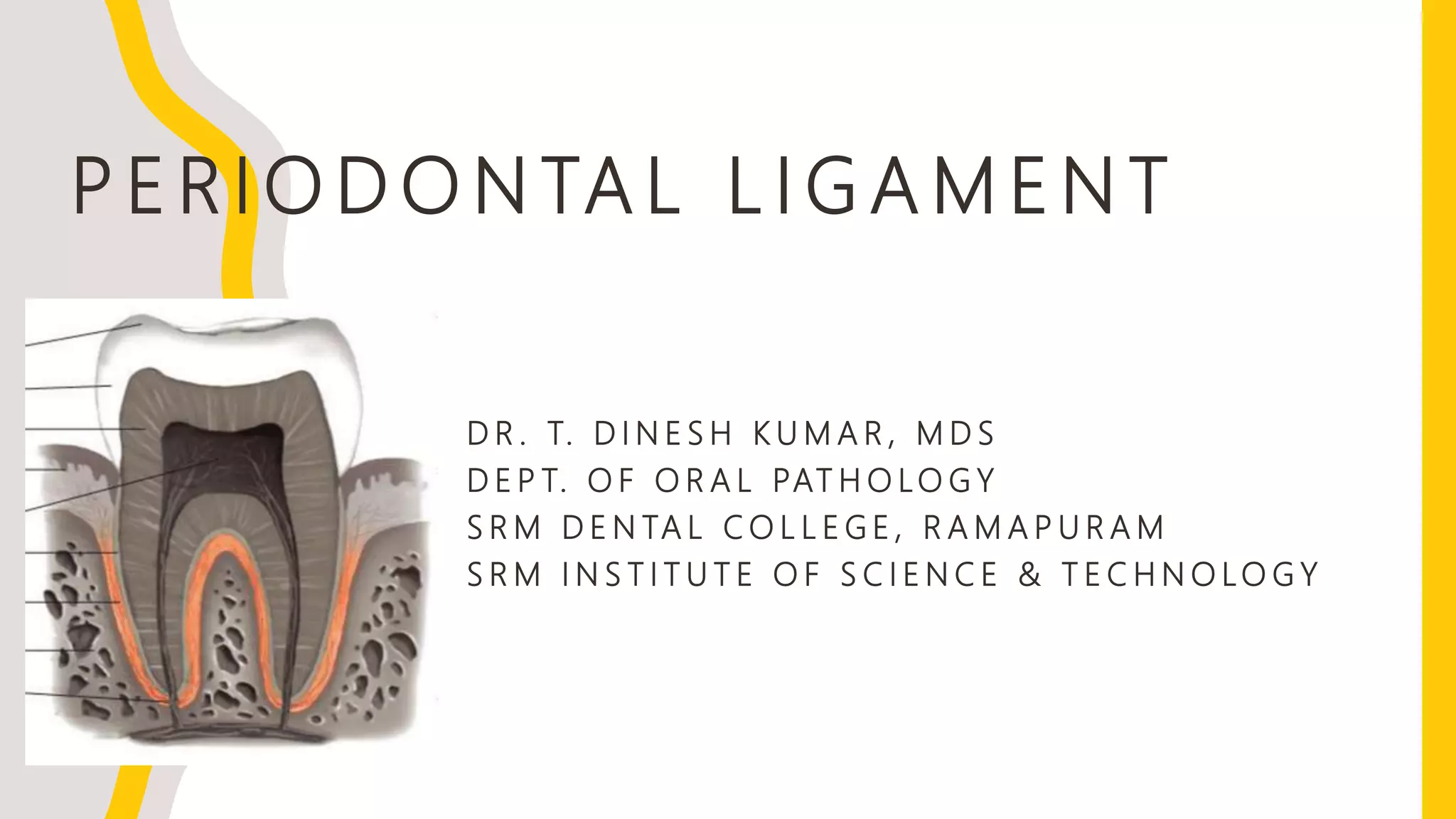
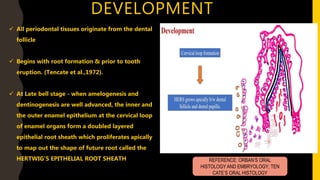
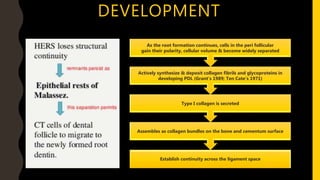
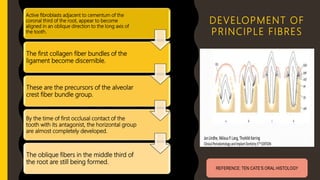
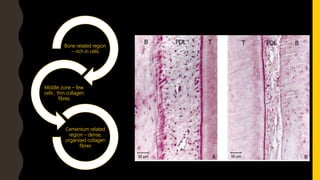
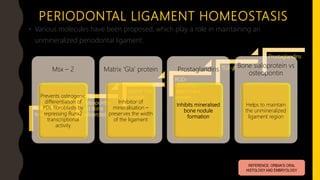
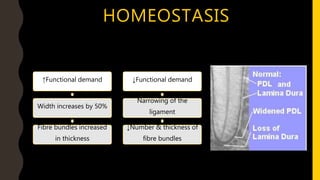
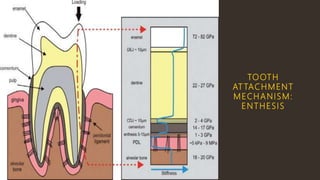
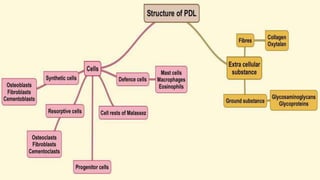
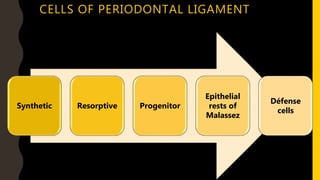
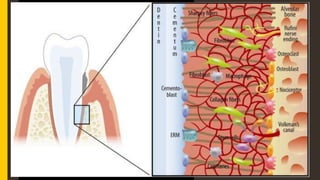
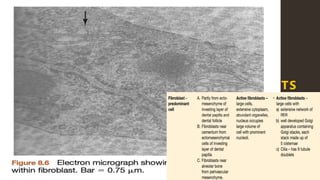
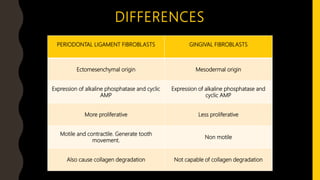
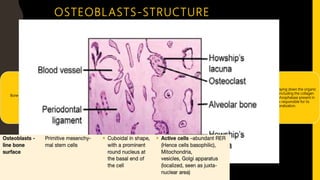
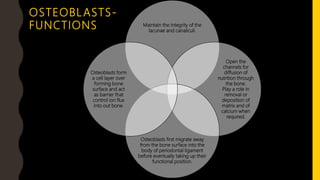
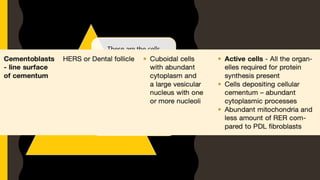
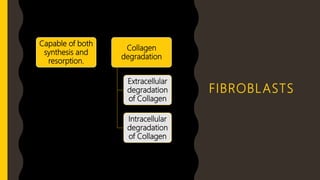
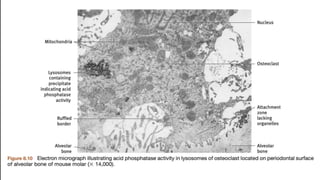
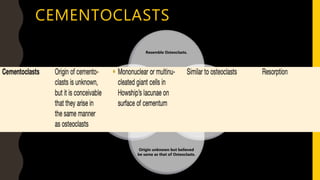
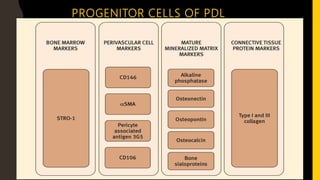
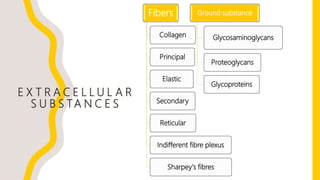
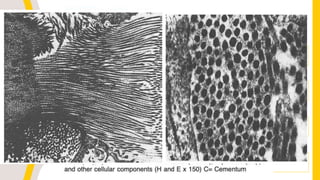
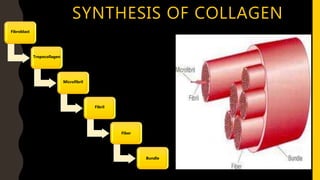
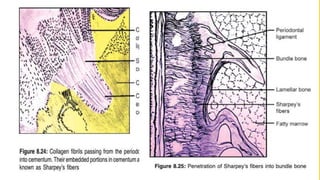
The periodontal ligament is a soft, vascular connective tissue that connects tooth roots to the alveolar bone socket. It develops from the dental follicle during root formation and tooth eruption. The periodontal ligament contains principal collagen fiber bundles oriented in different directions, as well as fibroblasts, cementoblasts, osteoblasts, and progenitor cells. It maintains homeostasis through a balance of synthetic and resorptive cells and extracellular substances. The unique structure and cellular composition of the periodontal ligament allow it to function in tooth attachment and as a sensory organ.