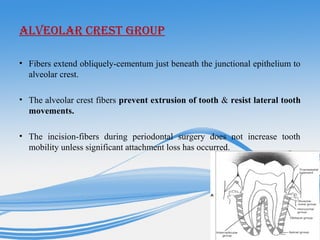
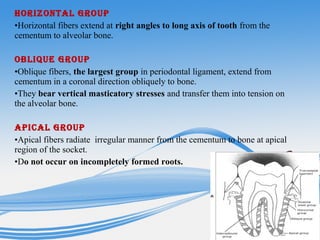
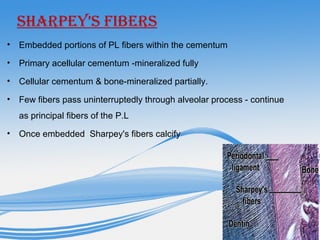
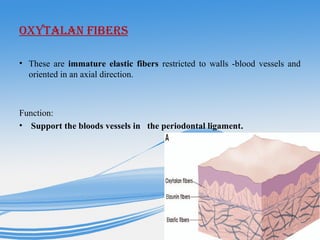
The periodontal ligament is a specialized connective tissue that connects teeth to the alveolar bone of the jaws. It is composed of cells, collagen fibers, blood vessels and nerves. The collagen fibers are arranged in bundles and attach to both the cementum covering the tooth root and the overlying alveolar bone. The periodontal ligament functions to attach teeth, absorb chewing forces, maintain the position of teeth, and allow limited tooth movement through the remodeling of its collagen fibers.