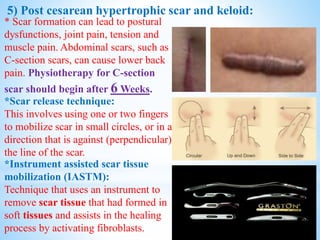
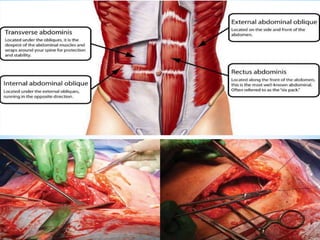
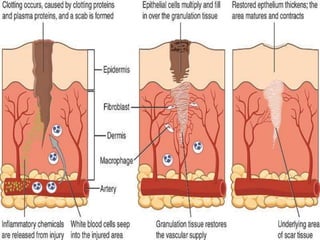
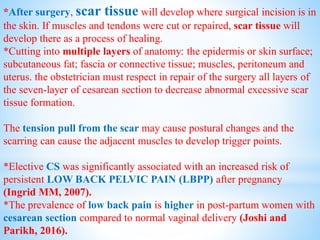
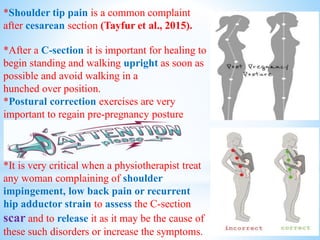
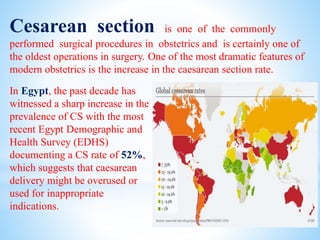
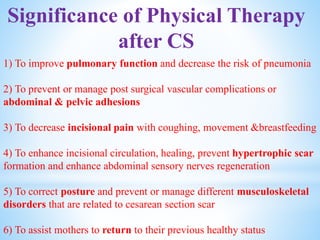
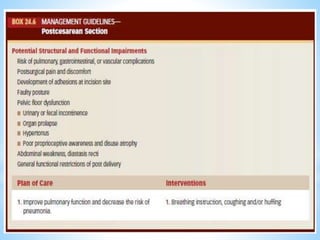
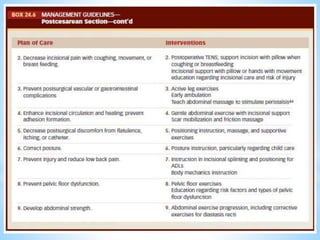
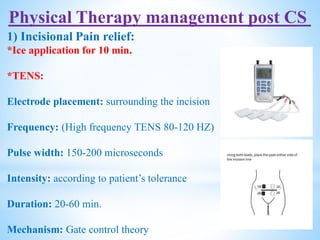
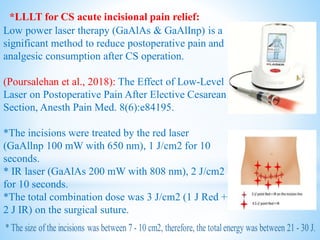
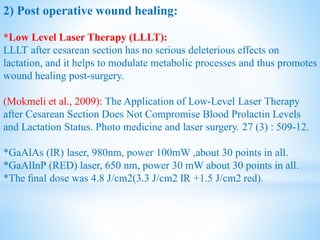
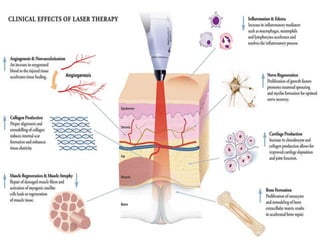
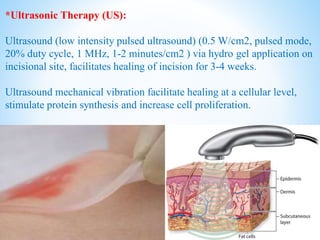
Cesarean section is a surgical procedure to deliver babies through incisions in the mother's abdomen and uterus. The rate of cesarean sections has increased sharply in Egypt in recent years. Physical therapy can help with pain relief, wound healing, reducing adhesions and numbness, and scar management. Techniques discussed include TENS, laser therapy, ultrasound, scar mobilization and more. Abdominal scarring from cesarean sections can impact posture and cause issues like low back pain, so physical therapy is important for recovery.





![*High Voltage Pulsed Galvanic Stimulation (HVPGS):
Voltage: always ranged from 150 to 200 V.
Intensity: The stimulation intensity was at a sensory level to prevent the
occurrence of motor reactions.
Pulse duration: 50-100 microseconds.
Frequency:100 HZ
Duration: 45-60min.[3 sessions weekly non infected & daily if infected]
Electrode placement: treatment electrode was placed on the wound with
dispersive electrode on healthy skin at least 15–20 cm from the wound.
Polarity: begin with negative treatment electrode to stimulate wound
healing if infected wound &positive treatment electrode if not infected.](https://image.slidesharecdn.com/cesarean-section1-200401215529/85/Cesarean-section-26-320.jpg)