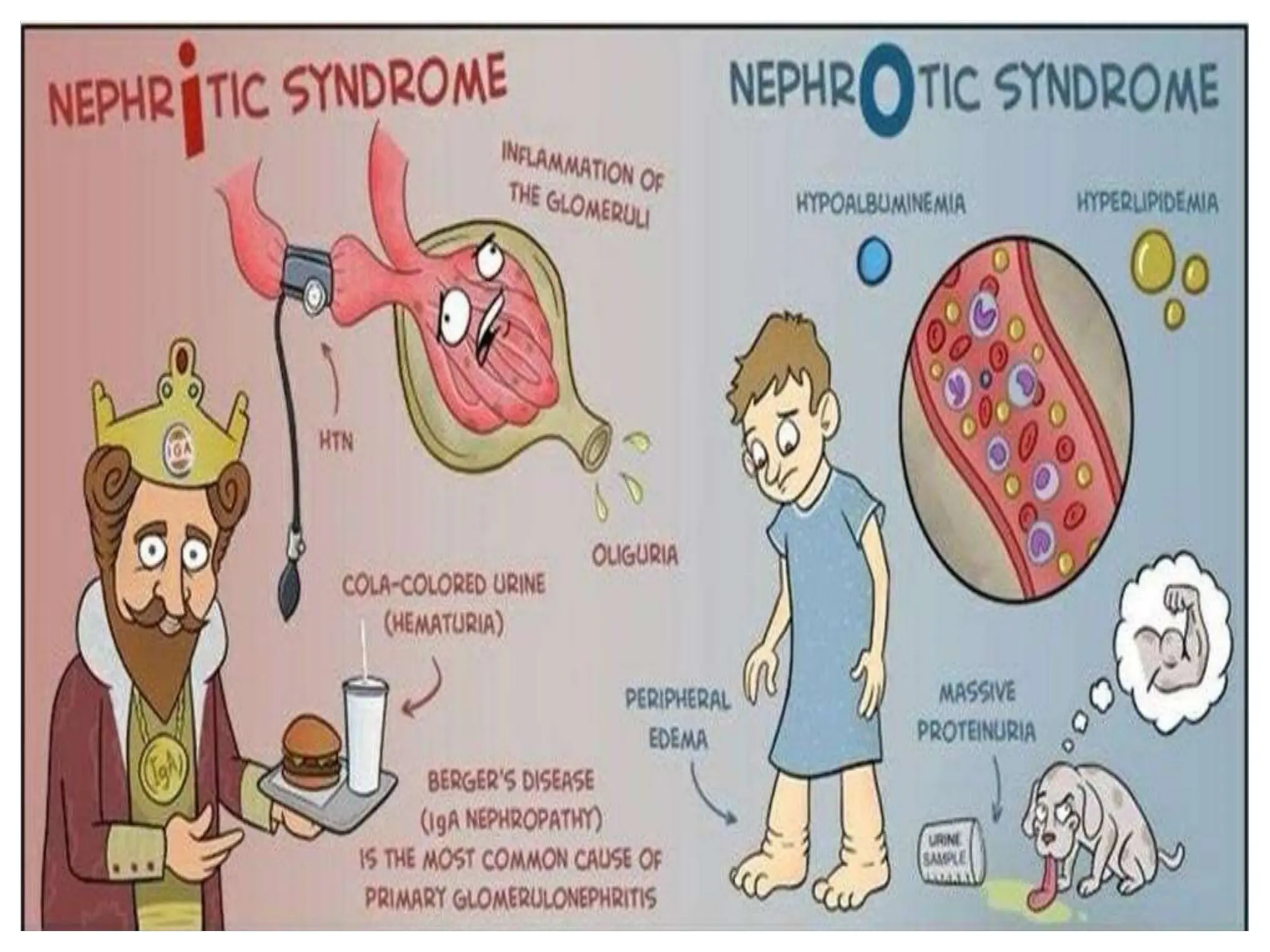
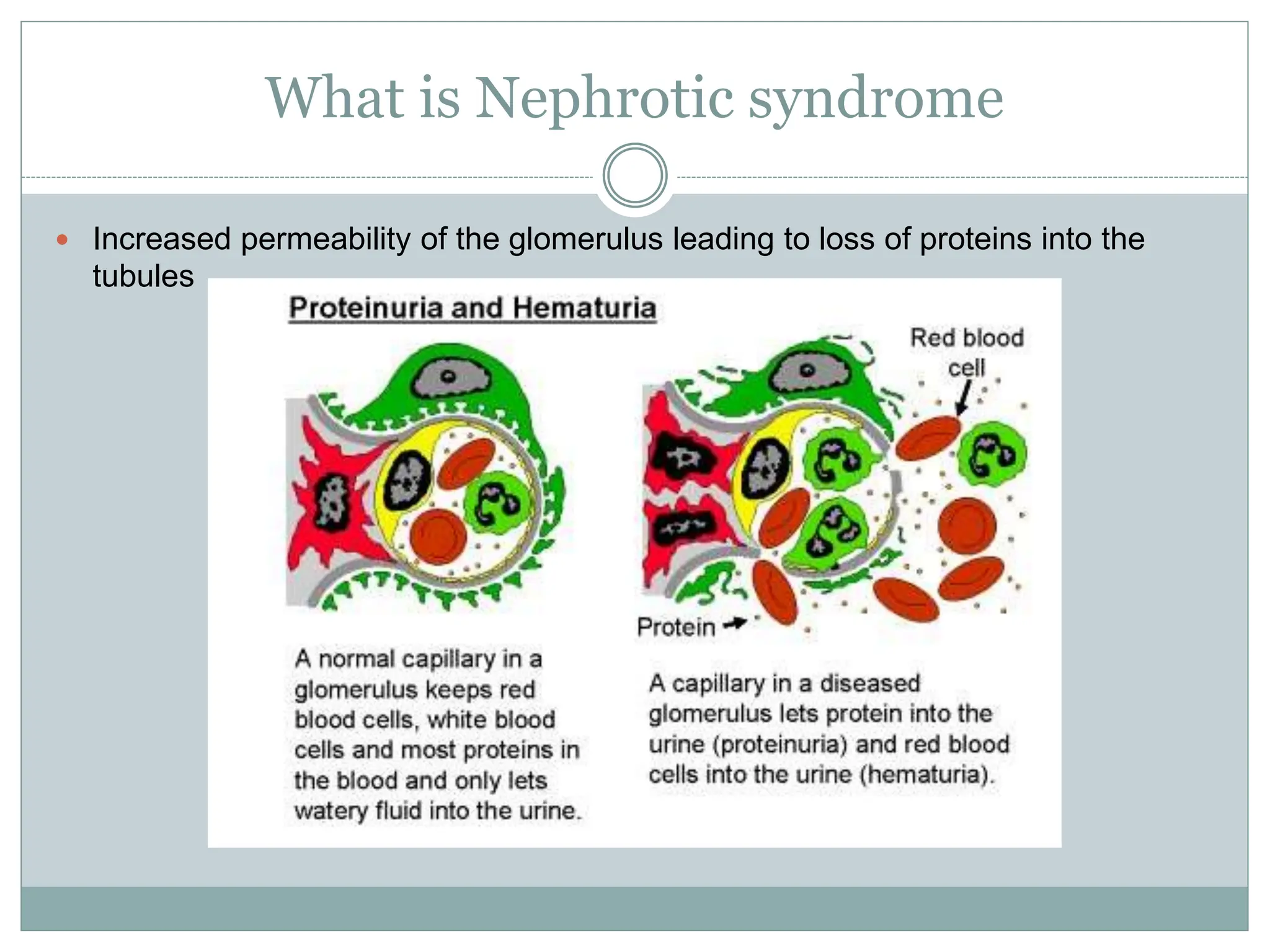
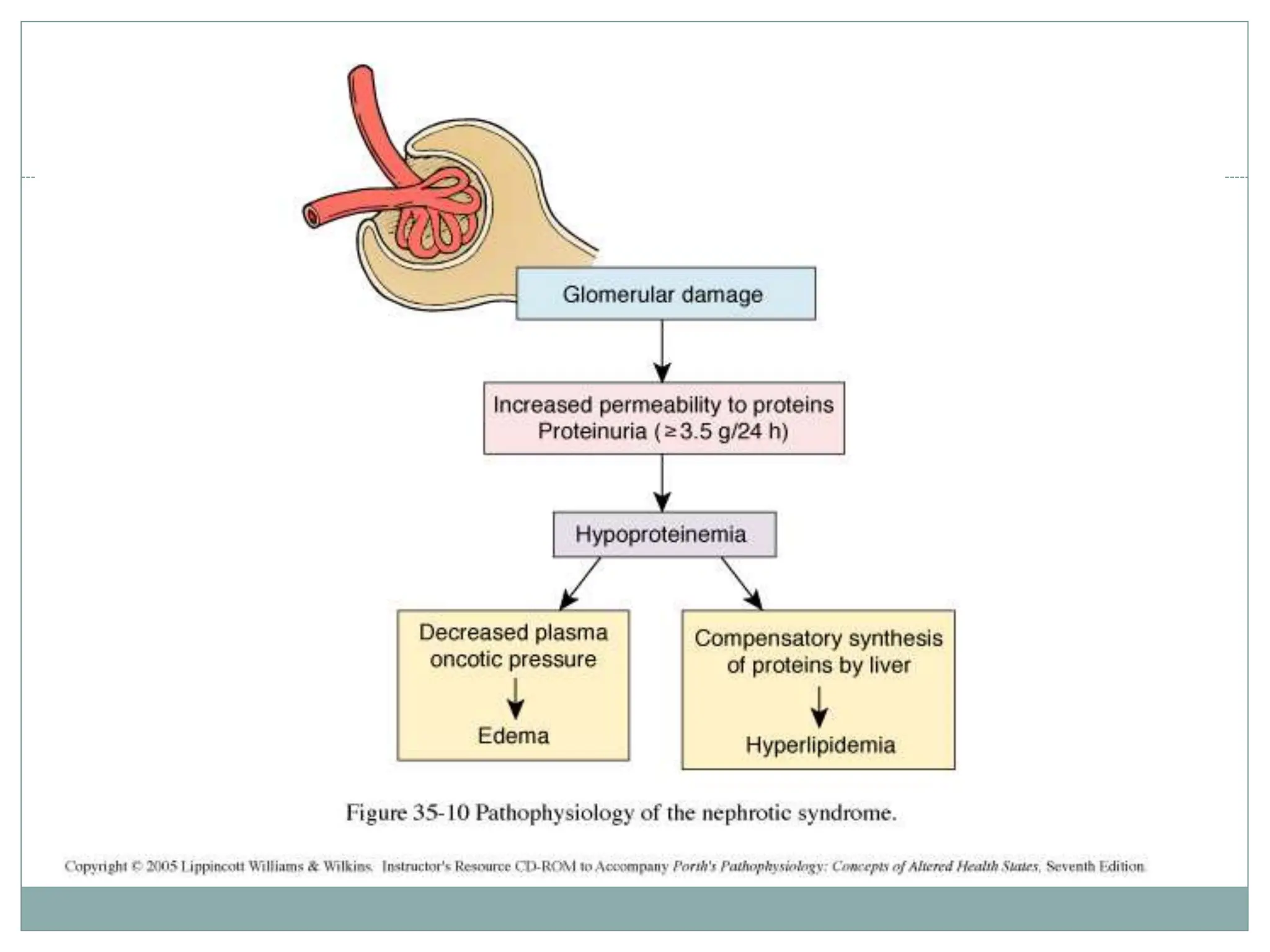
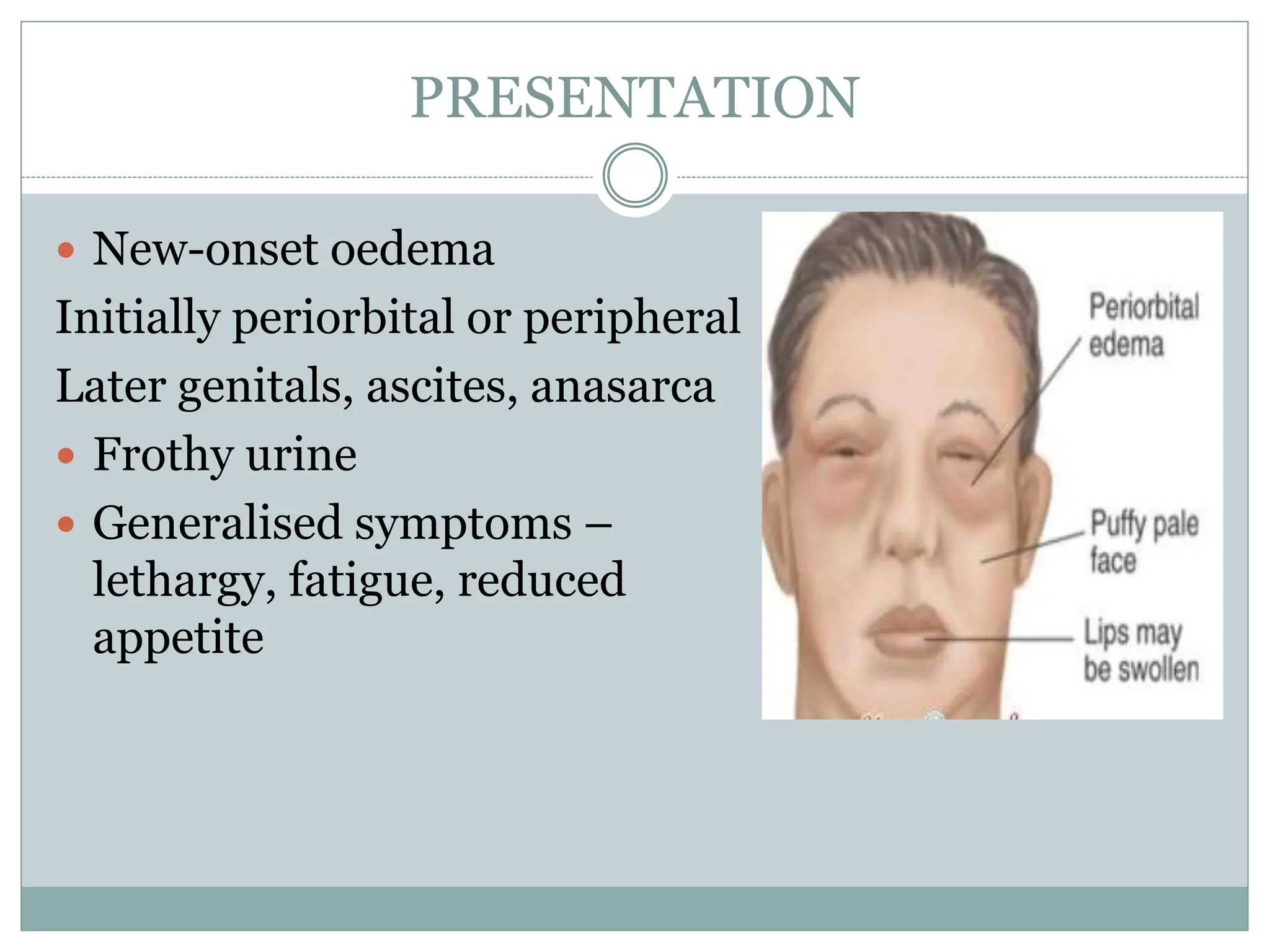
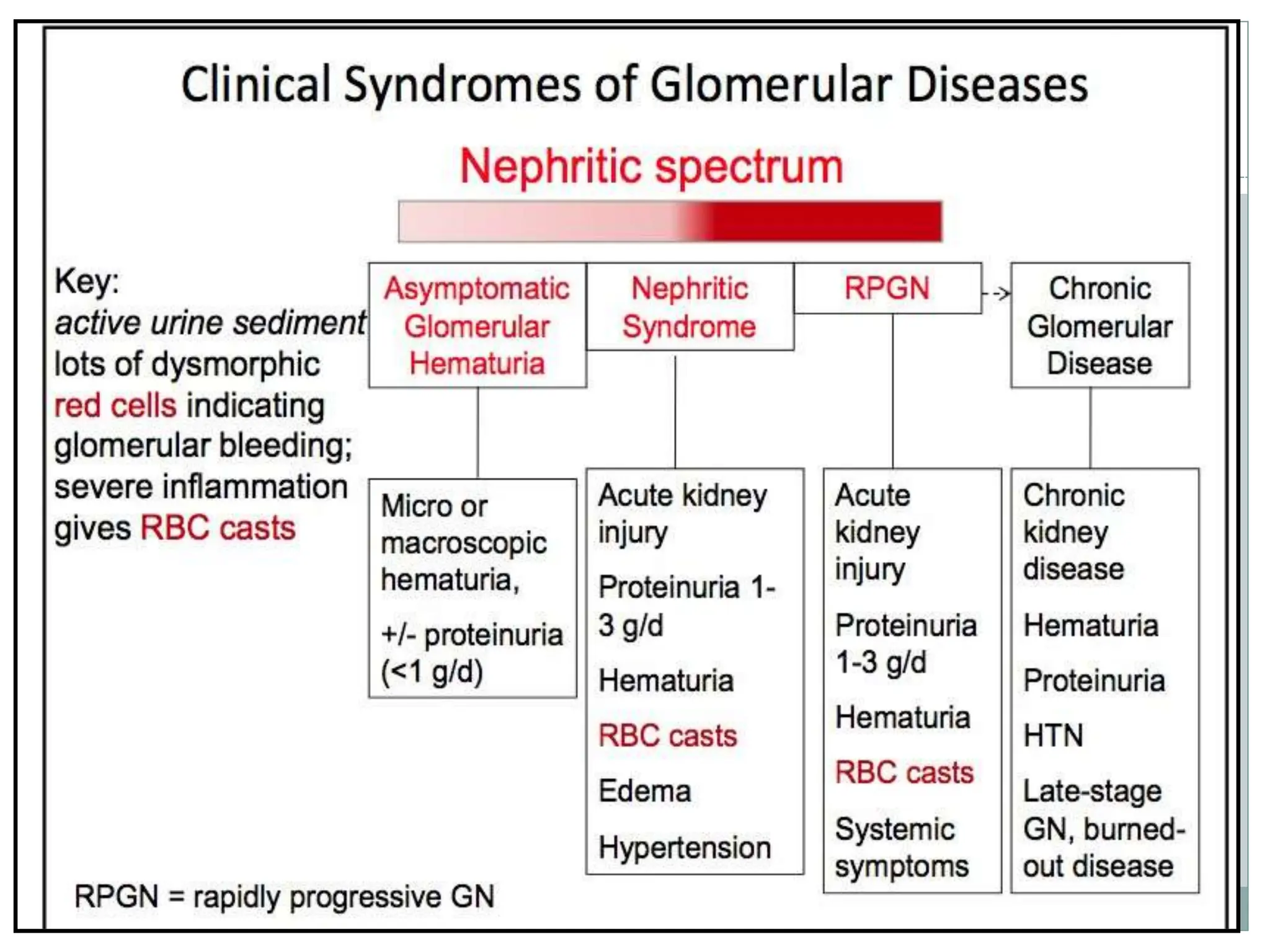
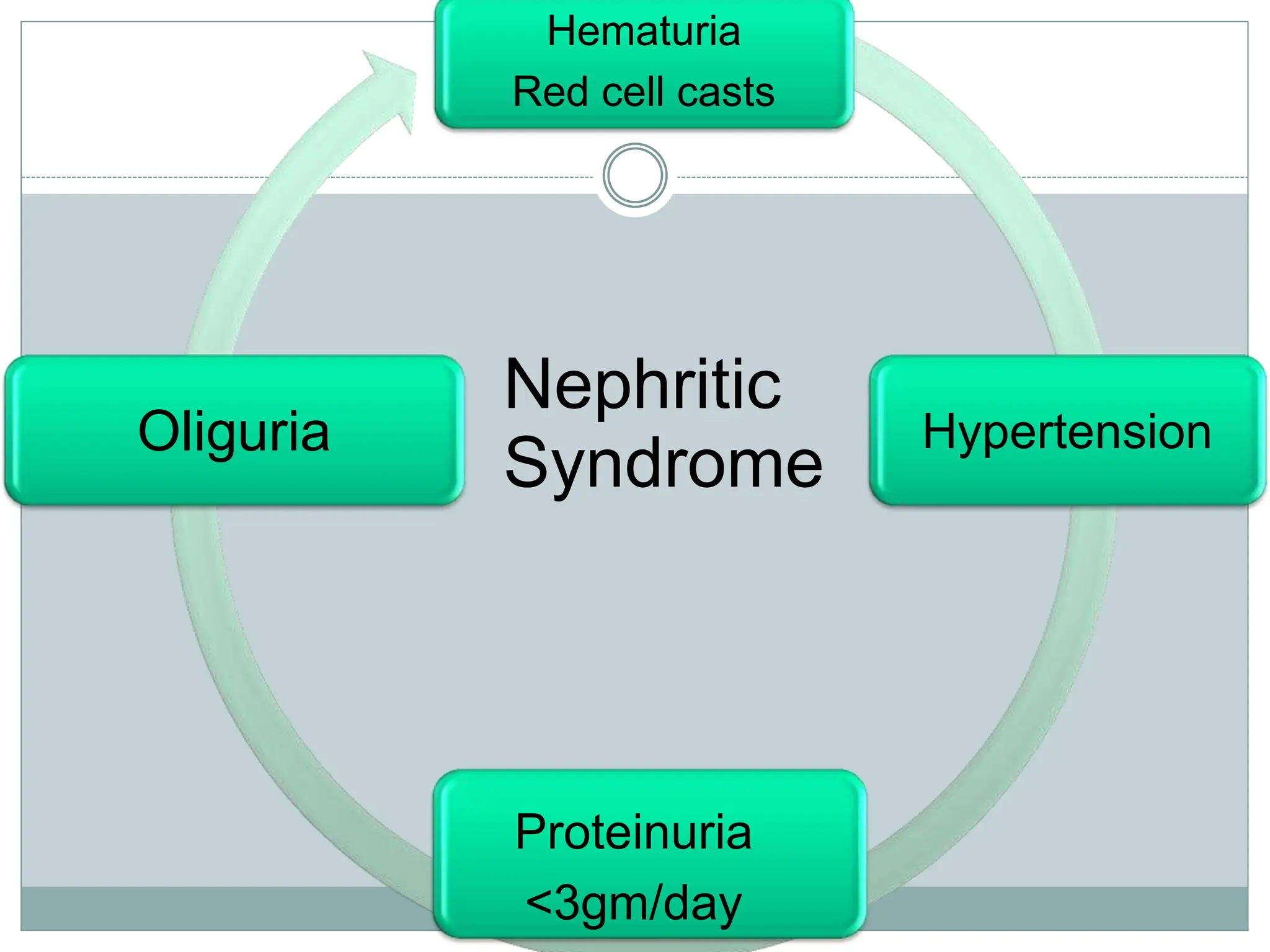
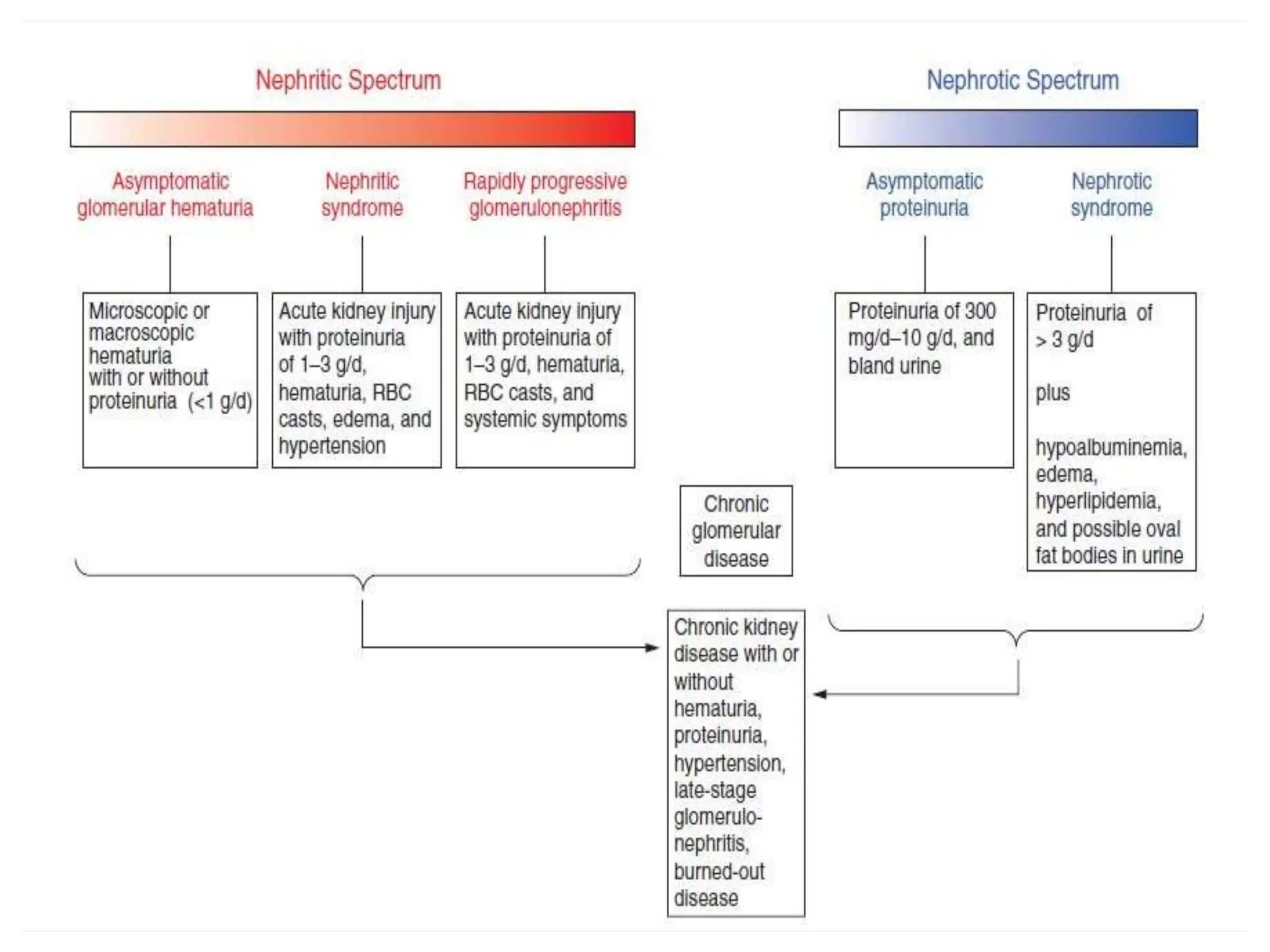
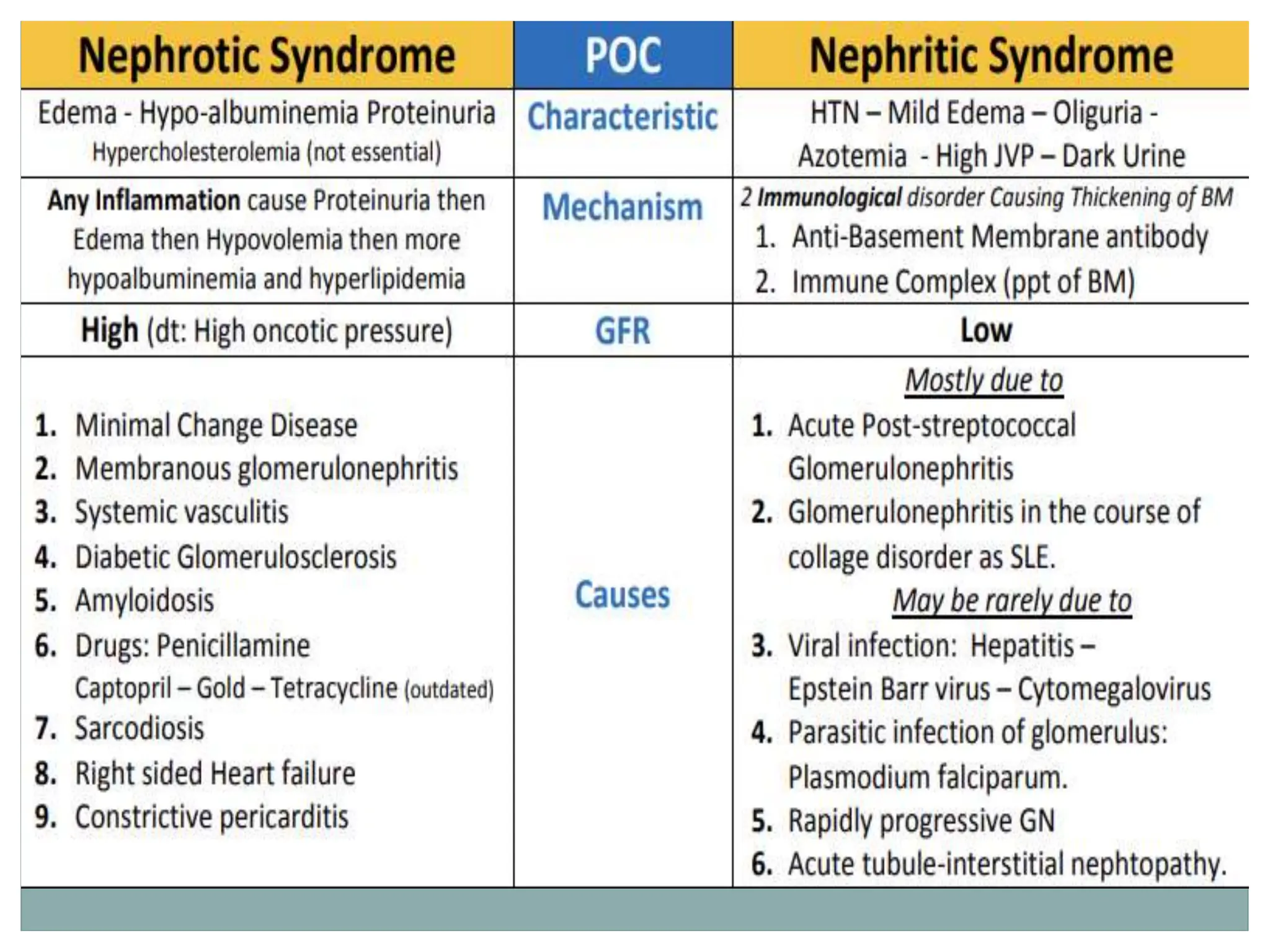
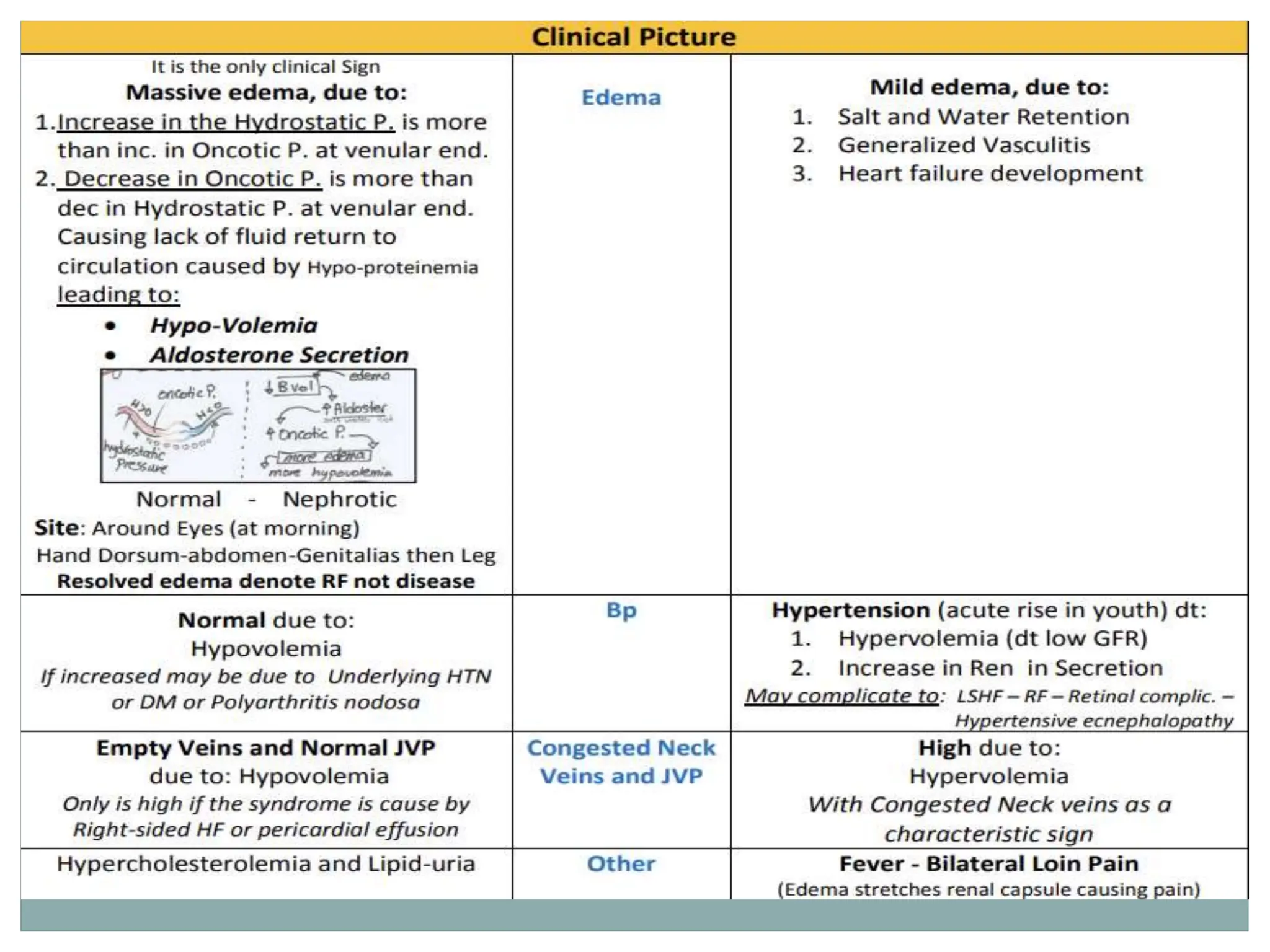
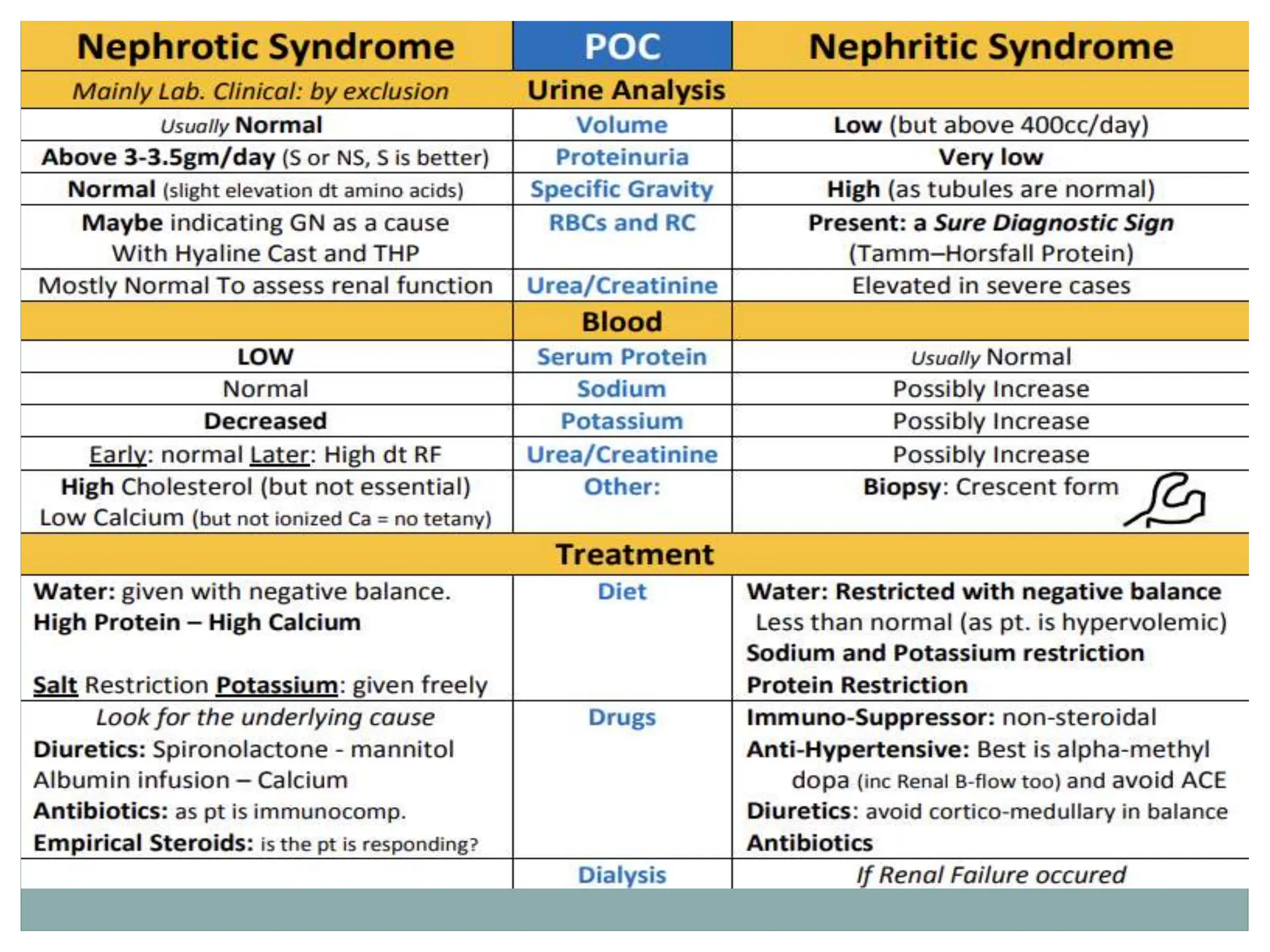
Nephrotic syndrome is characterized by massive proteinuria, hypoalbuminemia, and edema. It results from increased permeability of the glomerular basement membrane. Nephritic syndrome involves inflammation of the glomeruli that causes hematuria, hypertension, and sometimes reduced kidney function. While nephrotic syndrome presents with proteinuria and edema, nephritic syndrome presents with hematuria and red blood cell casts with proteinuria generally less than 3g per day. Both require diagnostic tests including urine analysis, blood work, and often renal biopsy for diagnosis and management.