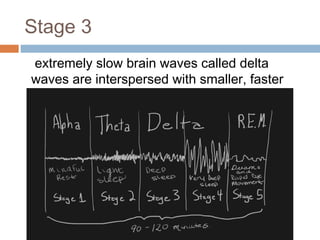
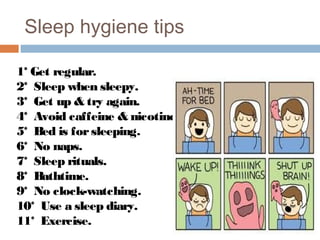
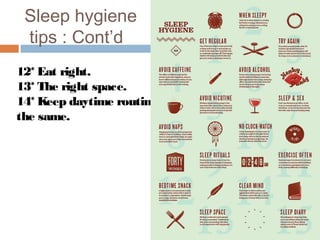
This document provides information about sleep disorders and sleep hygiene. It defines sleep and describes the stages of sleep including NREM, REM sleep, and the progression through stages 1-3. It discusses factors that affect sleep, consequences of poor sleep, and categories of sleep disorders like insomnia. Assessment of insomnia and interventions like CBT and medications are outlined. General sleep recommendations are provided regarding sleep schedules, environment, and habits. Sleep hygiene tips conclude the document.