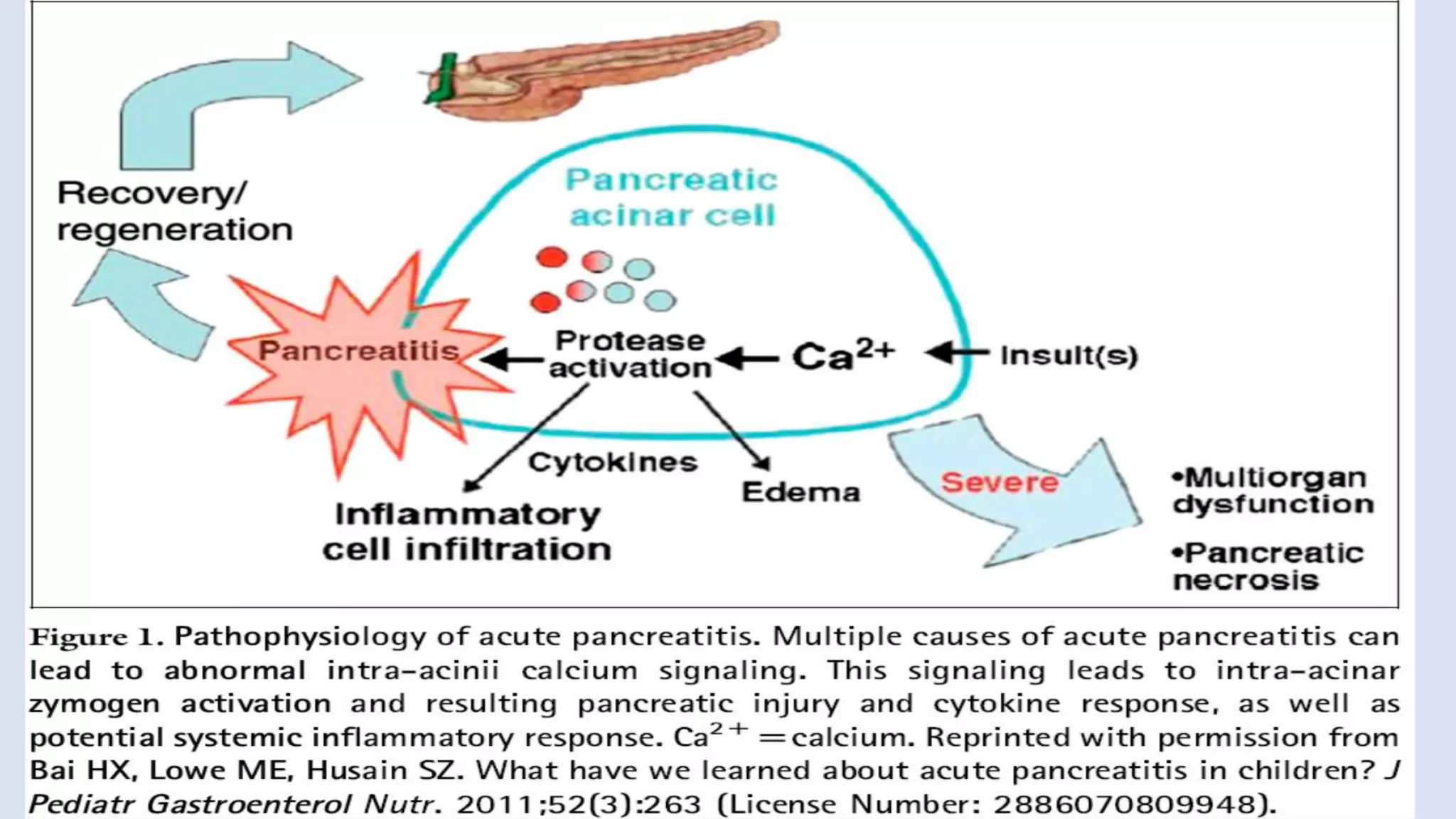
Pediatric pancreatitis is an inflammatory condition of the pancreas that can be classified as acute or chronic, with notable differences in etiology, presentation, and management between children and adults. Acute pancreatitis can arise from various causes including biliary disorders, infections, and genetic predispositions, while chronic pancreatitis results in irreversible damage and requires a multifaceted approach for diagnosis and treatment. Management strategies focus on supportive care, addressing underlying causes, and monitoring for complications, as the outcomes in children tend to be more favorable compared to adults.