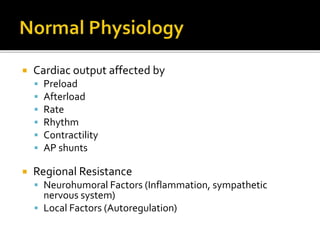
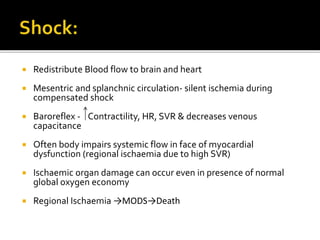
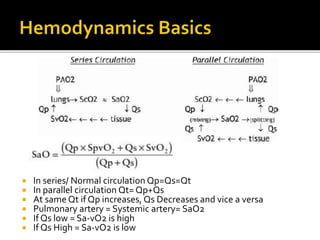
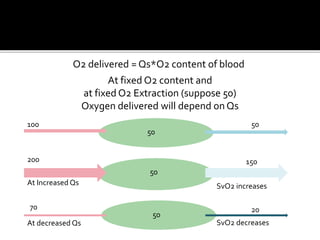
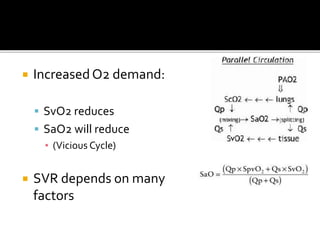
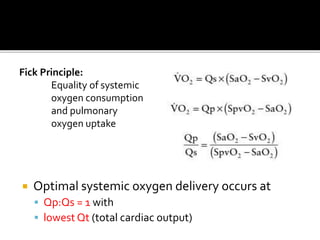
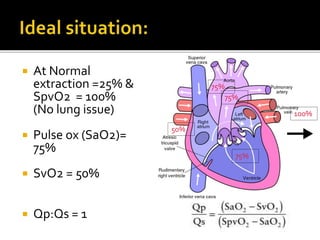
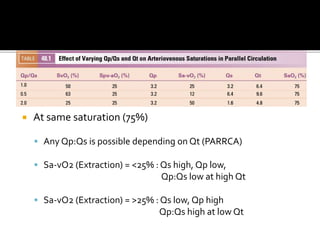
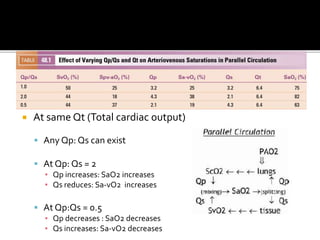
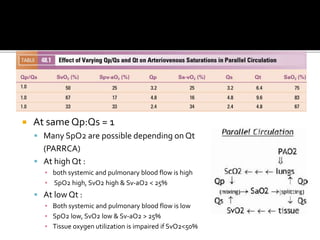
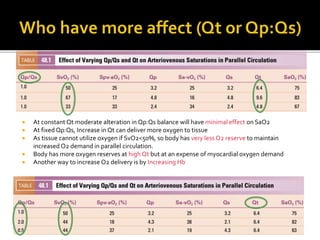
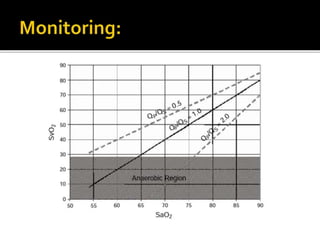
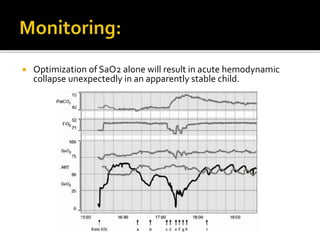
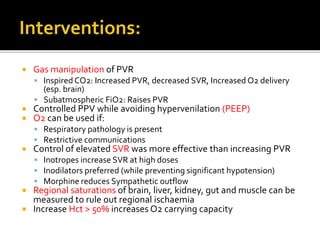
This document discusses cardiovascular physiology concepts related to cardiac output, blood flow distribution, and oxygen delivery and utilization in the body. It covers topics like the factors that affect cardiac output, regional resistance factors, blood flow redistribution, and the relationships between cardiac output, blood flow ratios in the pulmonary and systemic circulations, oxygen saturation levels, and oxygen delivery. The key ideas are that optimal oxygen delivery occurs at a pulmonary to systemic flow ratio of 1, with the lowest total cardiac output, and that subtle imbalances can significantly impact oxygen saturation and delivery levels.