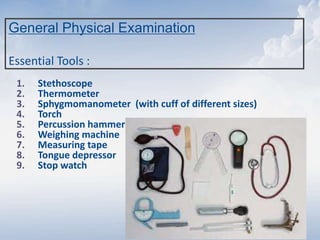
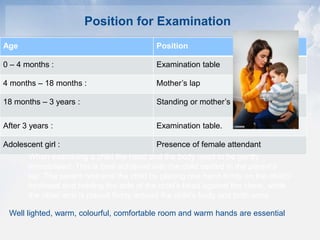
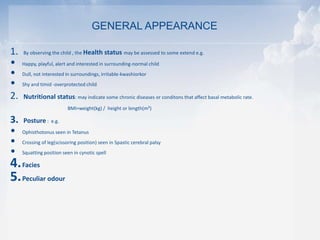
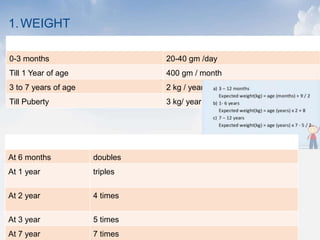
1. The document provides guidance on performing a general physical examination on children of various ages. It outlines the essential tools needed and the appropriate positioning for examination based on a child's age.
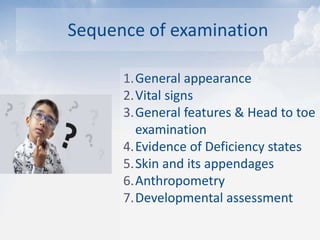
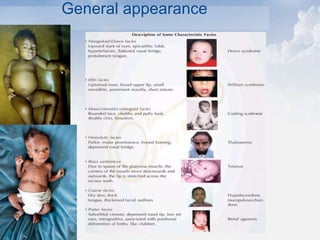
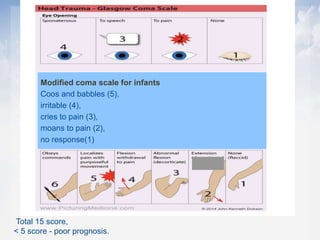
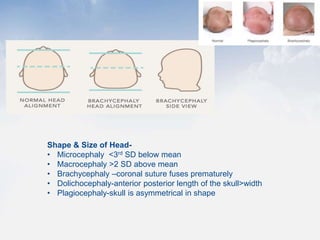
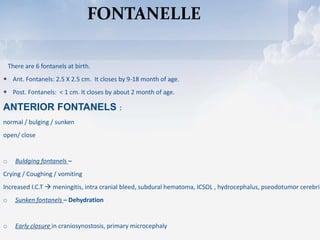
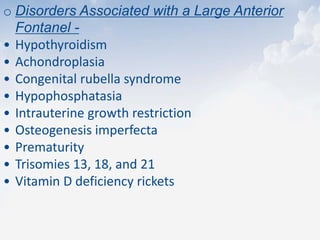
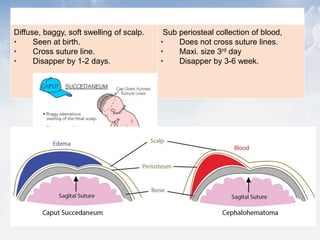
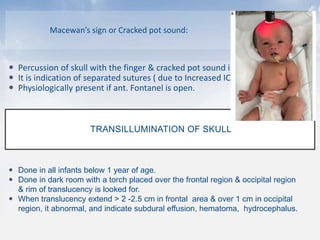
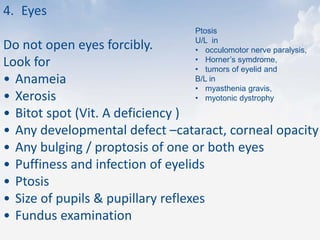
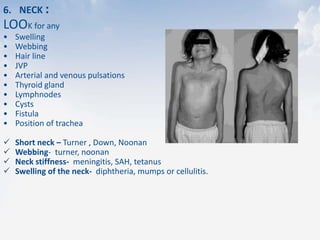
2. The sequence of examination is described, beginning with general appearance and vital signs, followed by examination of the head, eyes, ears, nose, mouth, neck, chest, abdomen, back, and extremities.
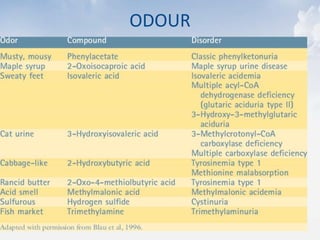
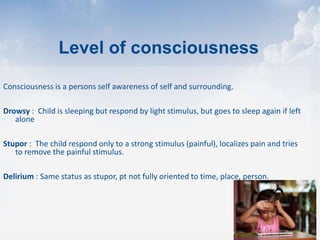
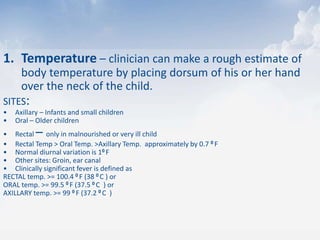
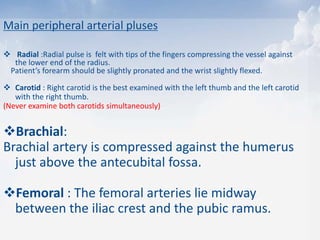
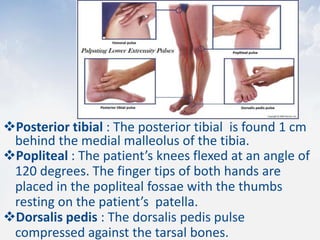
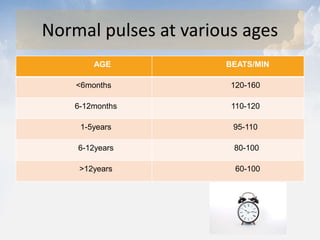
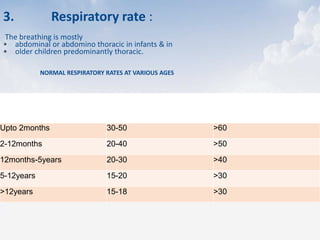
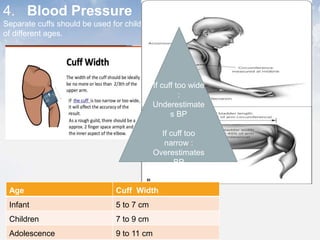
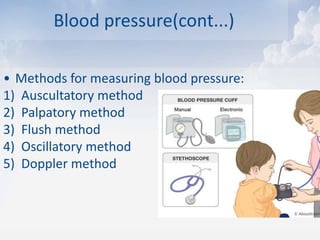
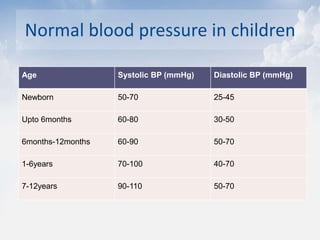
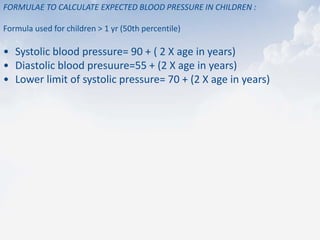
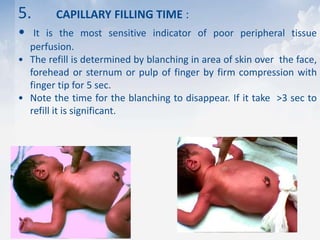
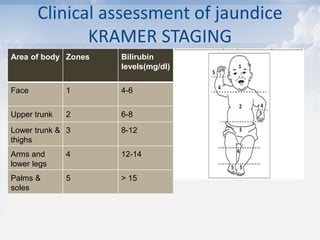
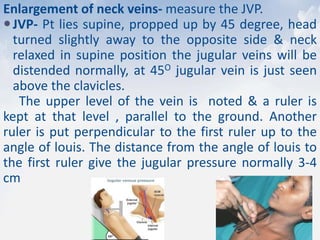
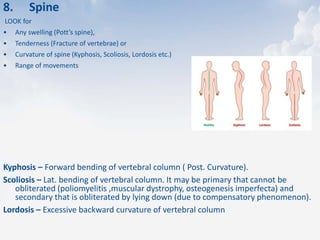
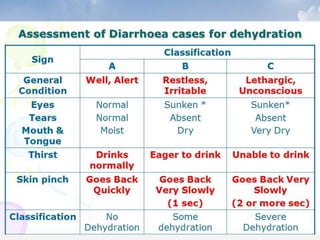
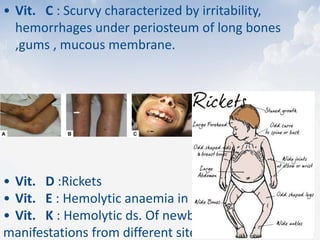
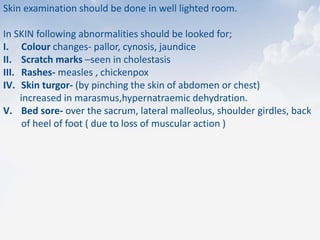
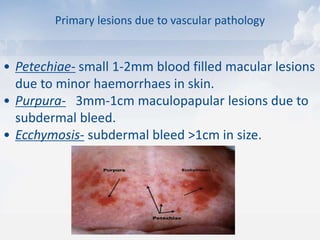
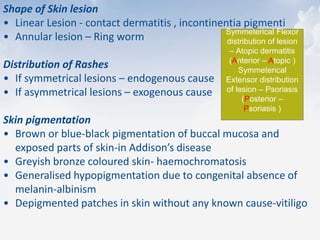
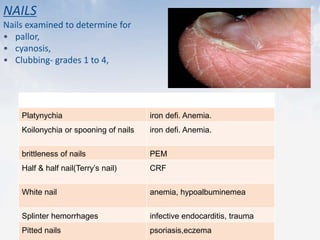
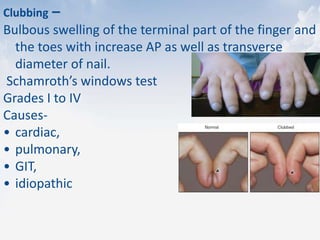
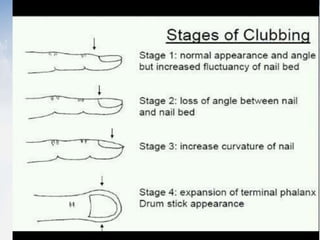
3. Specific assessments are outlined for various vital signs, including temperature, pulse, respiratory rate, and blood pressure. Guidance is also provided on examining general features, jaundice, edema, lymph nodes, and other body systems.