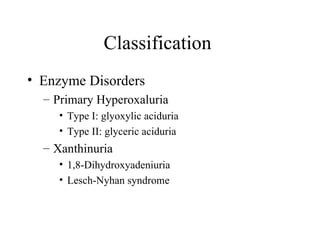
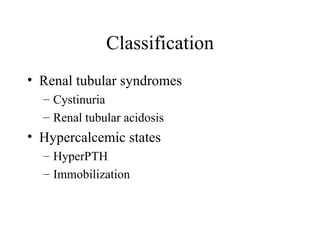
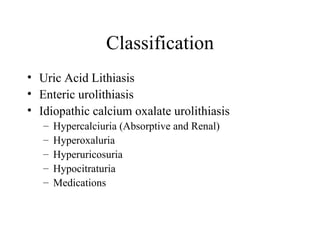
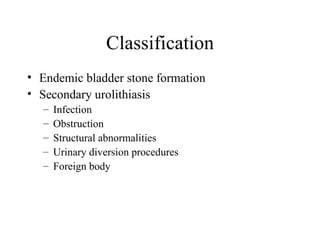
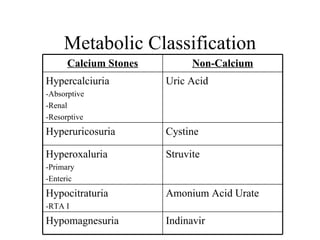
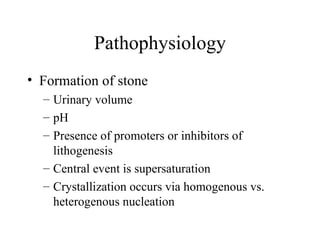
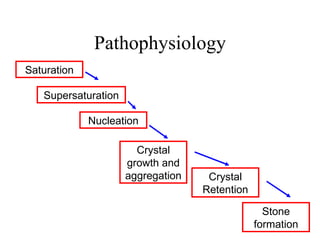
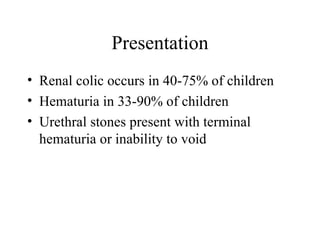
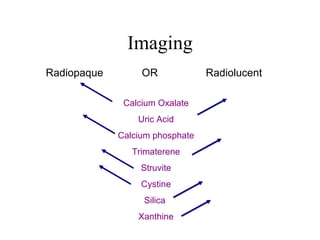
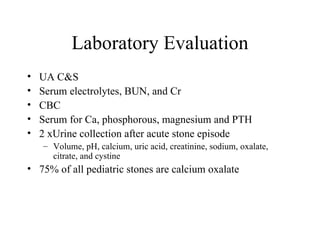
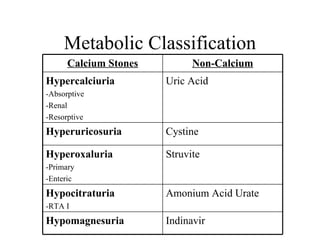
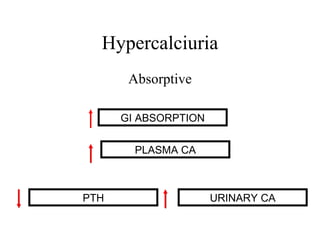
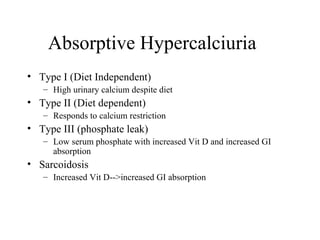
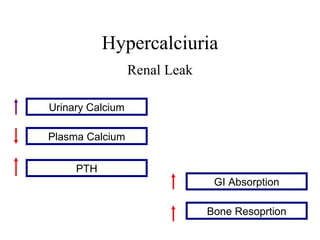
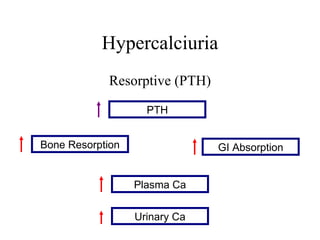
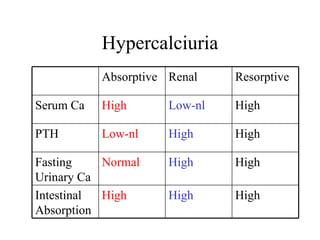
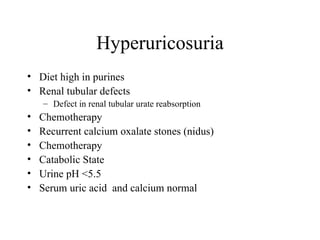
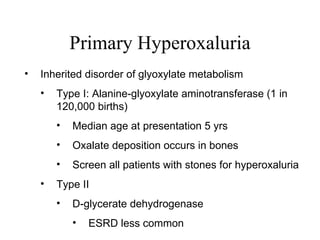
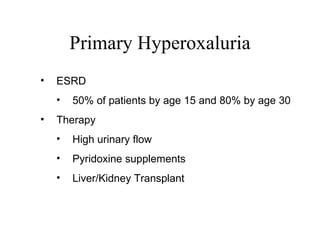
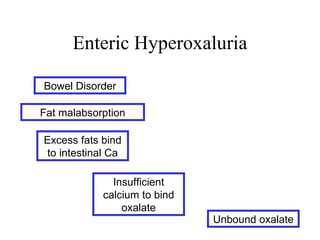
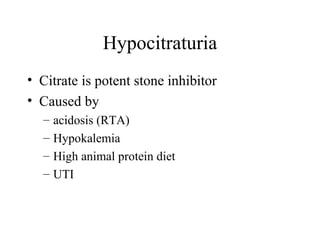
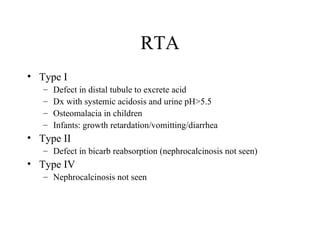
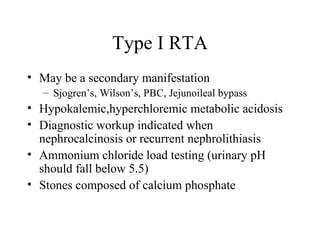
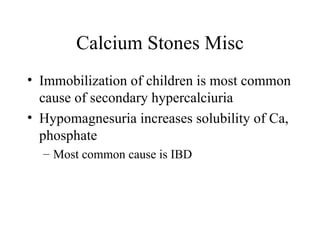
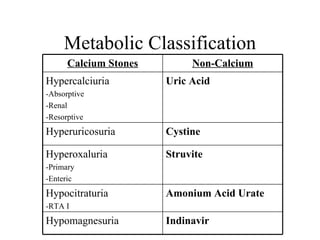
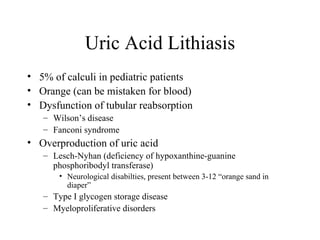
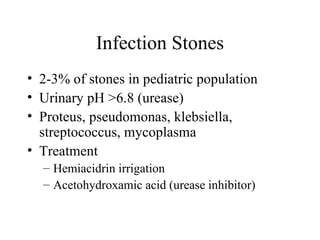
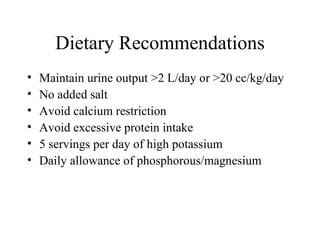
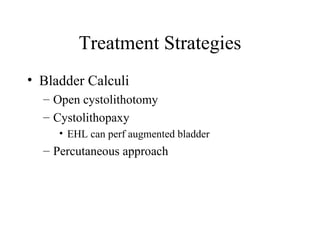
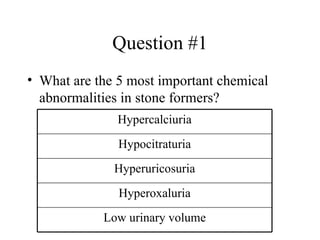
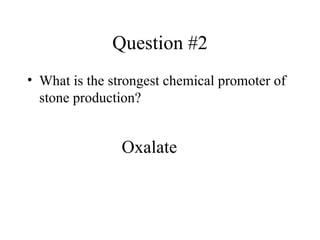
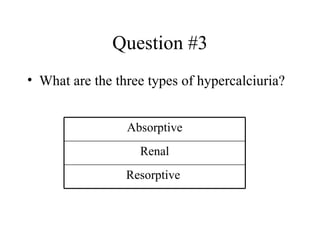
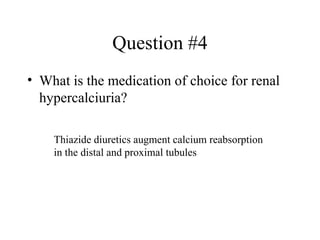
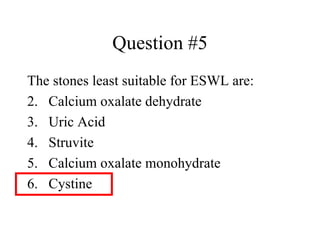
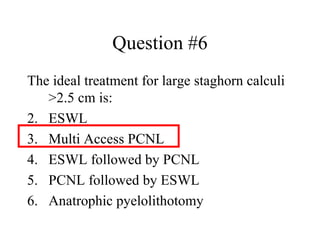
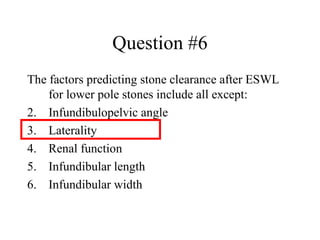
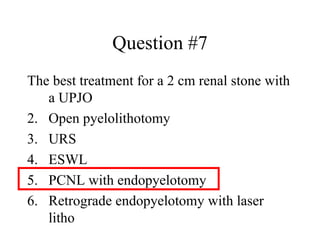
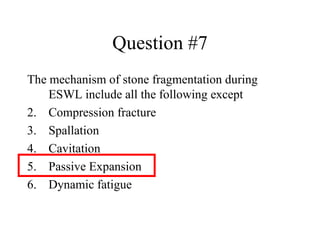
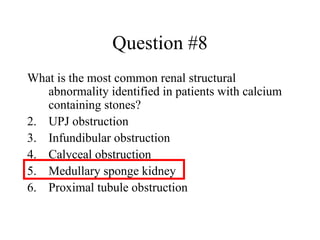
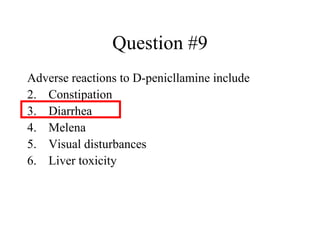
This document discusses the classification, pathophysiology, presentation, imaging, laboratory evaluation and treatment of nephrolithiasis in pediatric patients. The main types of stones include calcium, uric acid, cystine and struvite. Important risk factors are hypercalciuria, hypocitraturia, hyperoxaluria and low urine volume. Treatment depends on stone size and location but may include extracorporeal shock wave lithotripsy, ureteroscopy, percutaneous nephrolithotomy or open surgery. Diet and medical management target the underlying metabolic abnormalities promoting stone formation.