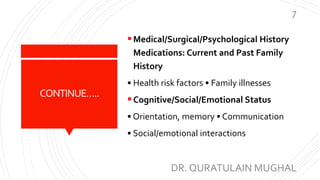
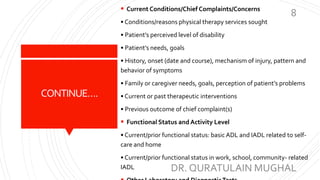
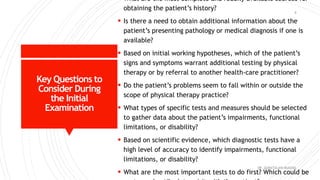
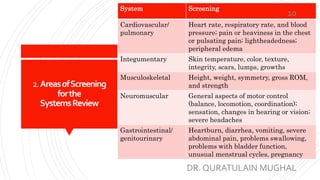
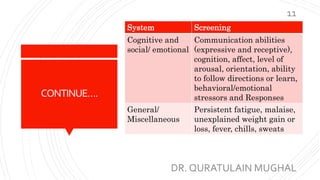
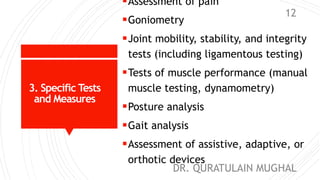
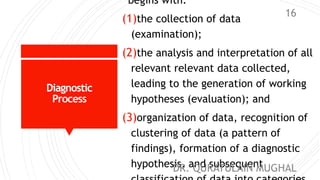
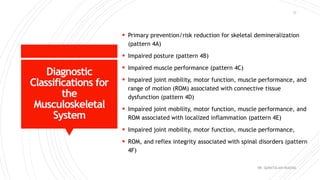
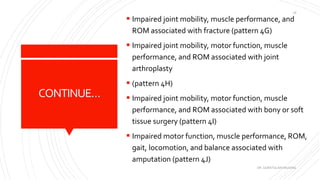
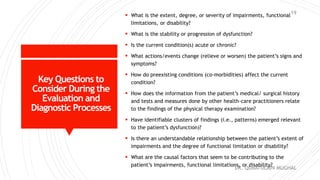
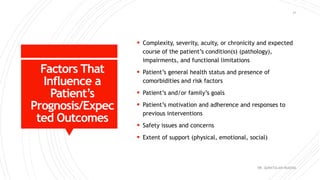
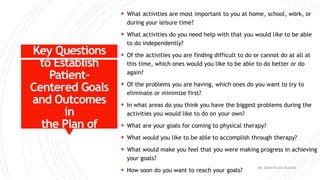
This document outlines the process of patient management in physical therapy. It discusses the key components of examination, evaluation, diagnosis, prognosis and care planning, intervention, and outcomes. The examination involves obtaining a health history, systems review, and specific tests to evaluate the patient's impairments, functional limitations, and disabilities. In the evaluation, the therapist analyzes and interprets the examination data. They then make a diagnosis, which can be a label or the diagnostic process. The prognosis predicts the patient's expected functional outcomes and time to achieve them. The care plan establishes goals and the interventions needed. The interventions directly work with the patient, and outcomes measure the results including the patient's function and satisfaction.