This document provides guidance on effective history taking in physiotherapy. It discusses:
- The importance of history taking for diagnosis, disease understanding, and physical exam focus. Trust and active listening are keys.
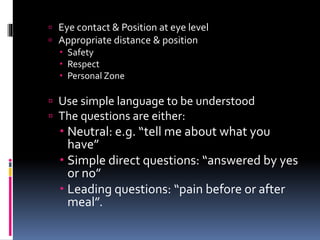
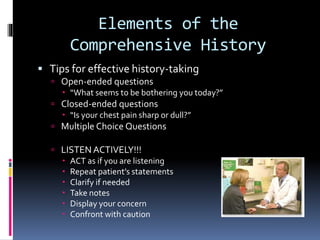
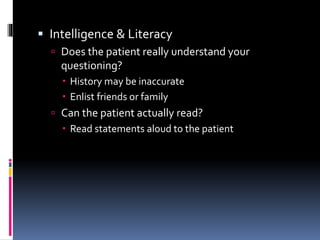
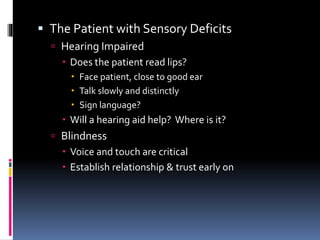
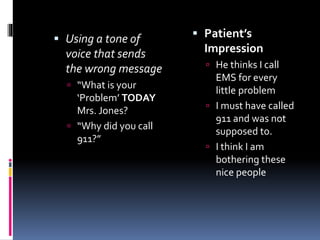
- General guidelines for history taking, including gaining patient confidence, using simple language, and asking open, closed, or leading questions.
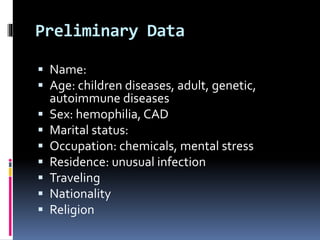
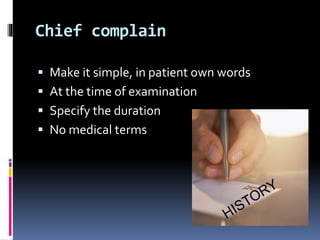
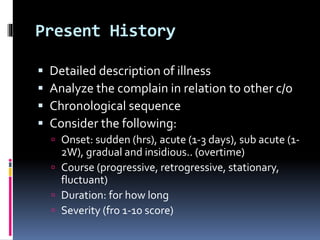
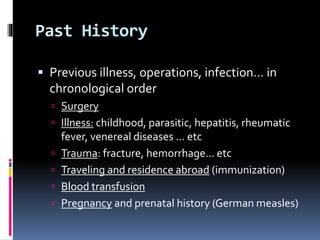
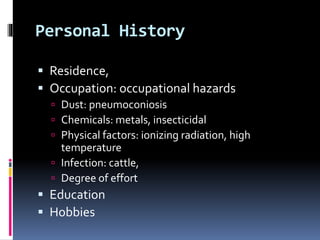
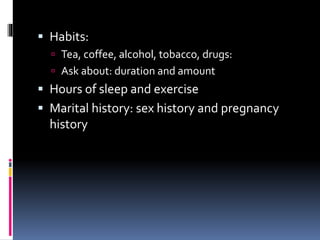
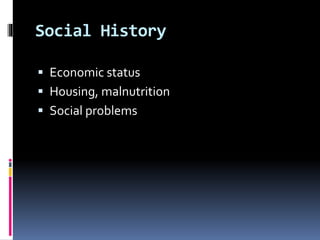
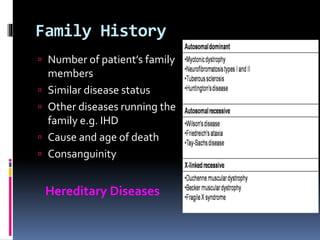
- Elements to cover in the history such as preliminary data, chief complaint, present and past history, social history, and family history.
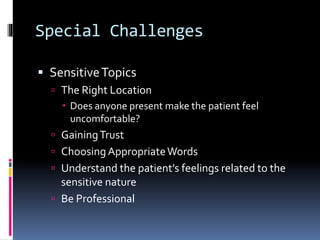
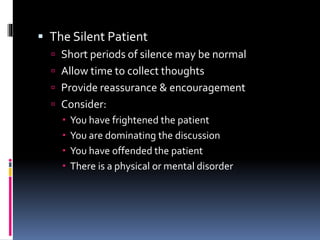
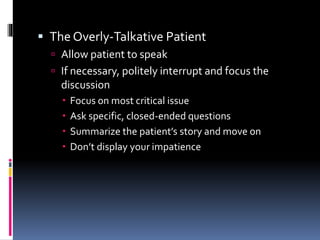
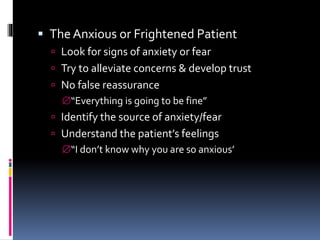
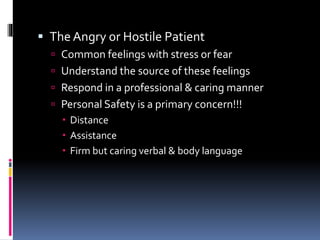
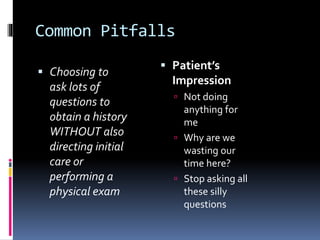
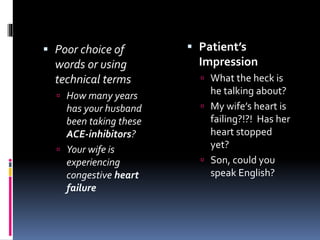
- Challenges such as sensitive topics, anxious patients, language barriers, and avoiding common pitfalls like disrespecting culture or using confusing terminology.
The overall message is that history taking is essential for physiotherapy, and