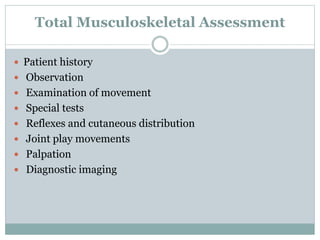
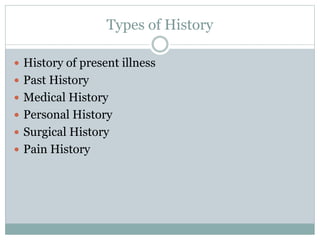
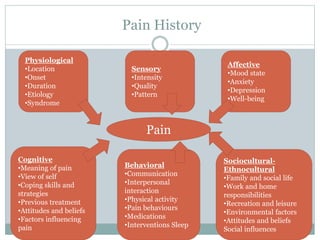
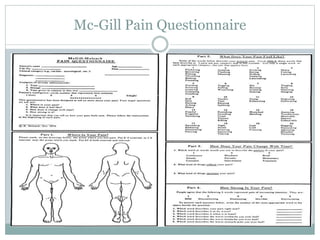
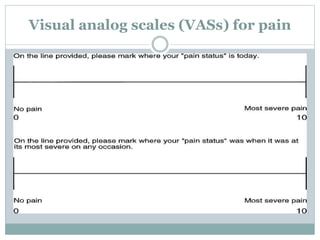
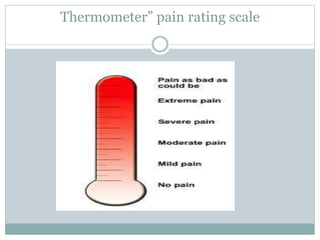
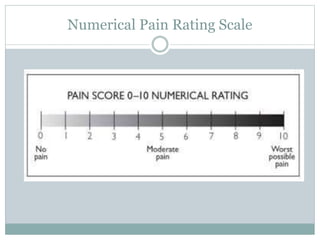
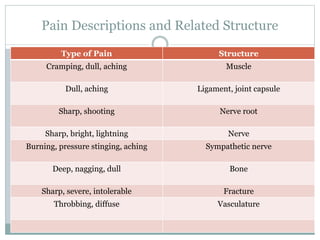
The document discusses the examination of musculoskeletal dysfunction. It explains that the examination involves both subjective and objective components. The subjective examination includes a thorough patient history, with details on types of histories to collect and pain scales to assess pain levels. The objective examination involves observing movement, performing special tests, assessing reflexes and sensation, and examining joint play and palpation. Both subjective and objective parts of the examination are needed to fully understand the patient's problem and make an accurate diagnosis.