Physiotherapy aims to prevent and treat impairments through physical examination, evaluation, diagnosis and intervention. It promotes mobility, functional abilities and quality of life. Physiotherapists assess, diagnose, treat and evaluate patients to restore optimal physical function and movement. Physiotherapy can benefit patients with orthopedic, neurological, cardiac, pulmonary, burns and many other conditions through techniques like exercises, modalities, manual therapy and airway clearance. It is commonly used to treat pain, increase range of motion and strength, improve balance and prevent complications from immobility.



























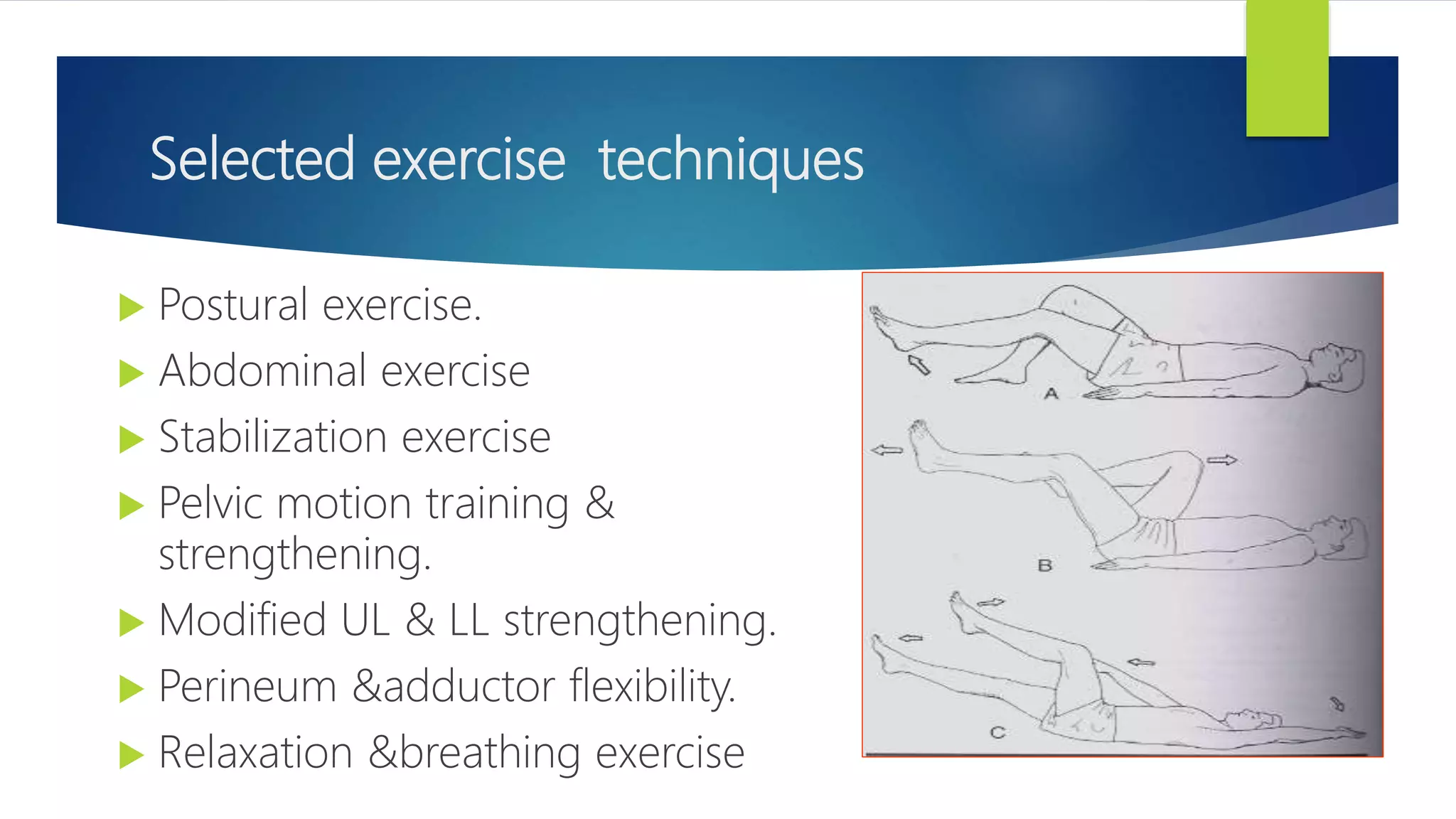
![Suggested sequence of exercise
General rhythmic activities to warm-up.
Gentle selective stretching
Aerobic activities for CVS conditioning
UL &LL strengthening ex.
Abdominal ex
Pelvic floor ex.
Relaxation /cool down activities
Educational information [if any] & postpartum ex. Education.](https://image.slidesharecdn.com/scopeofphysiotherapyipdandopd-201130111841/75/Scope-of-physiotherapy-ipd-and-opd-32-2048.jpg)