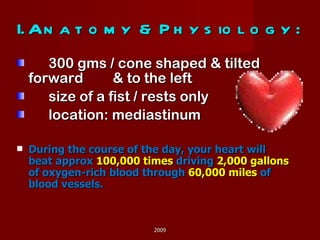
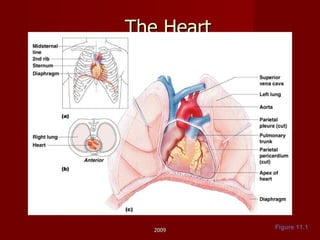
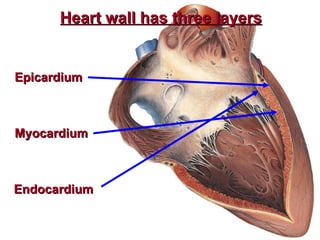
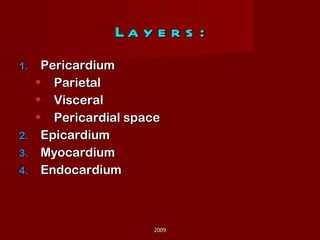
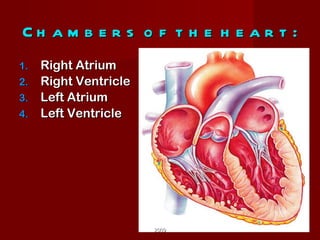
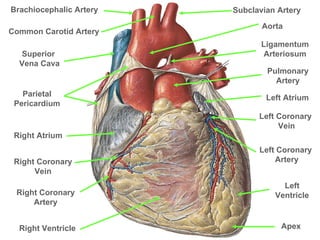
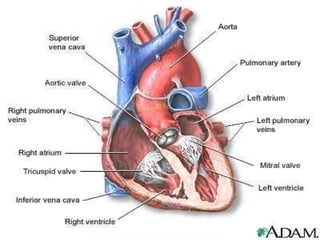
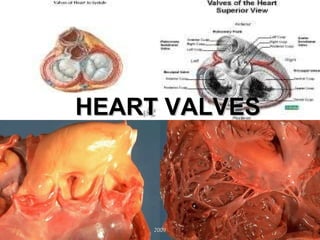
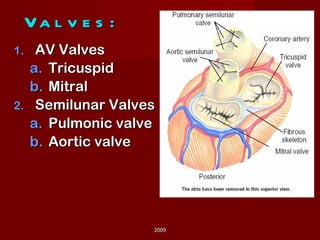
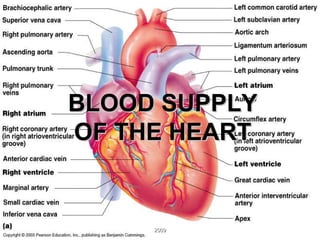
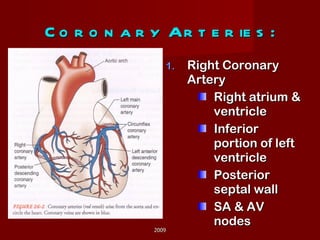
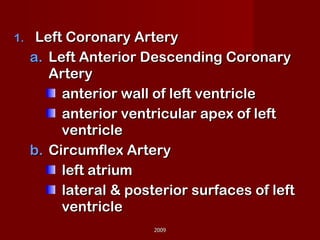
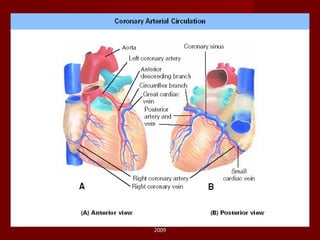
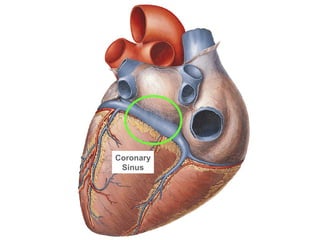
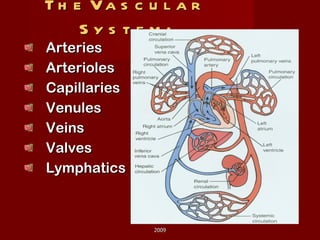
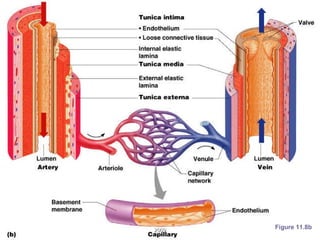
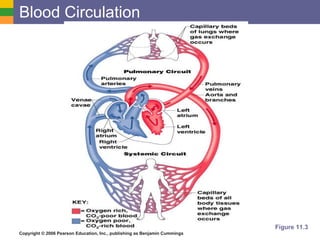
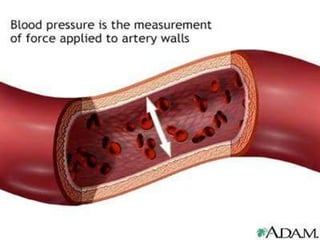
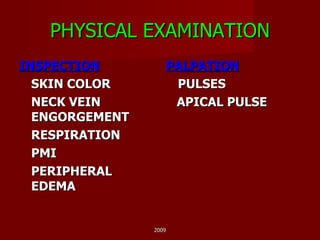
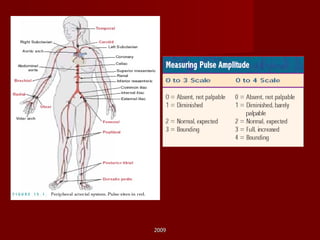
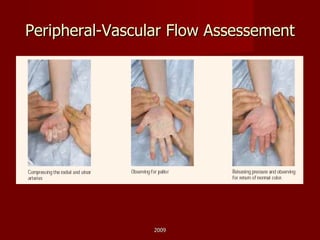
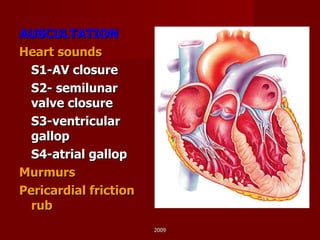
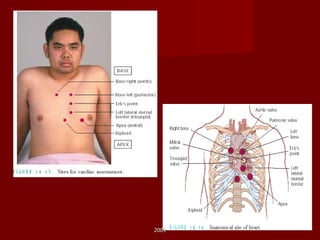
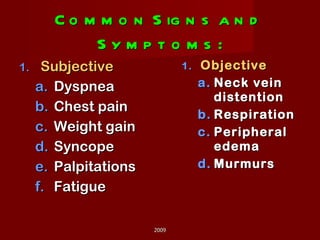
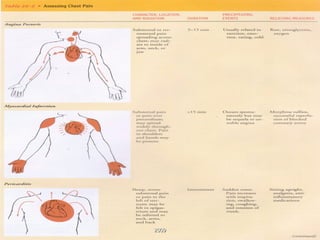
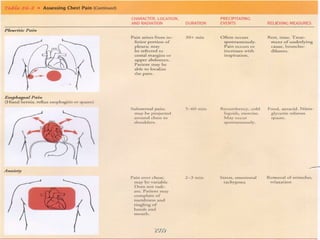
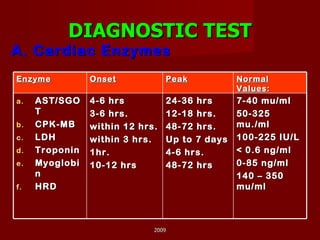
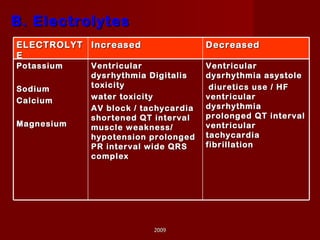
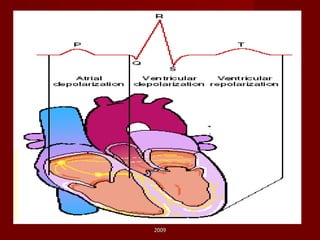
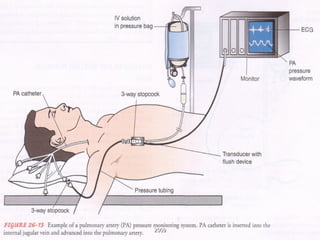
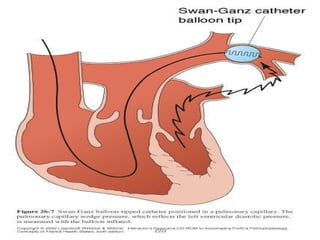
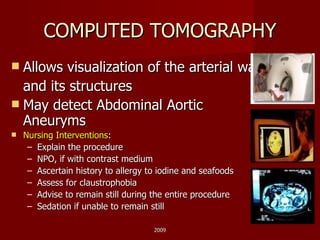
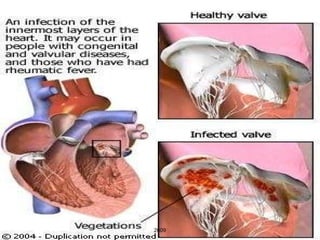
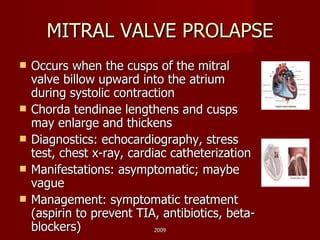
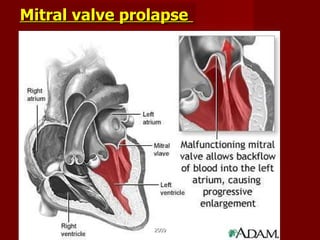
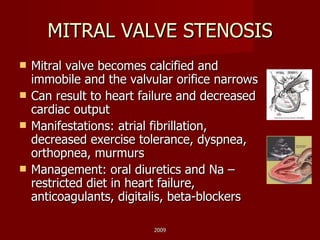
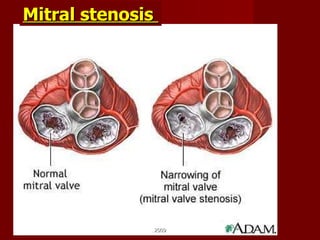
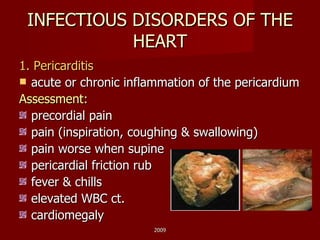
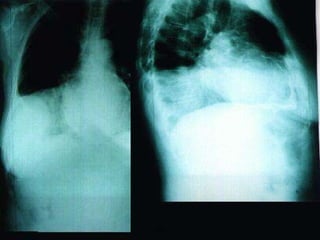
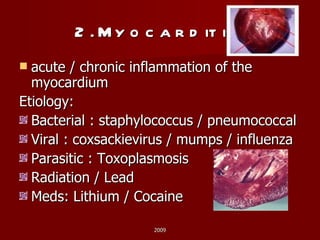
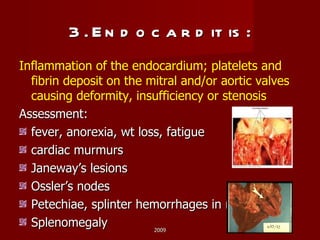
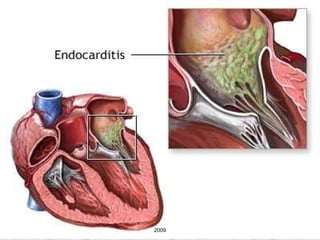
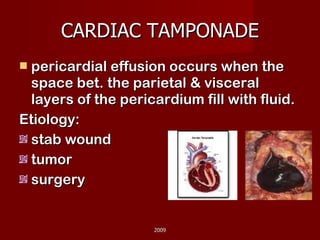
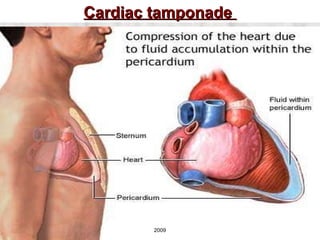
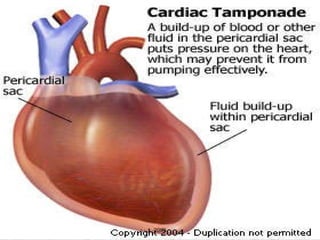
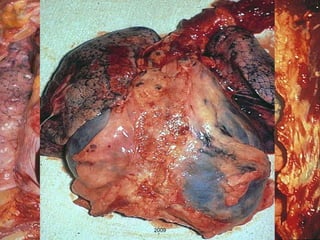
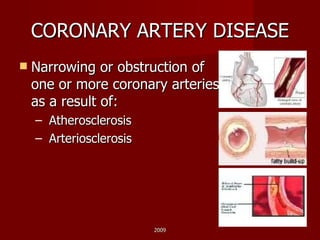
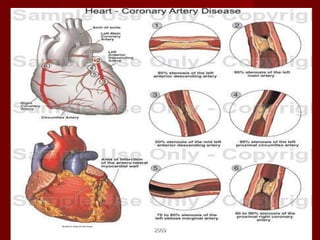
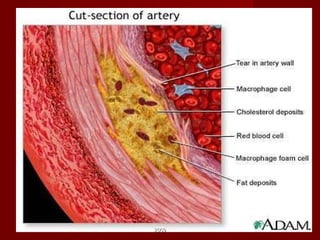
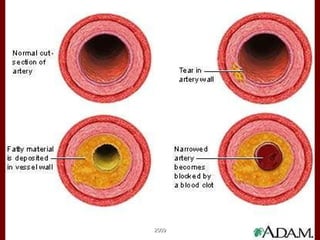
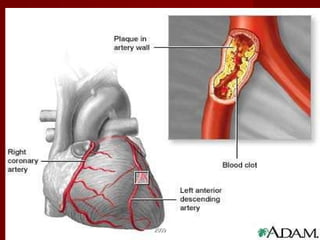
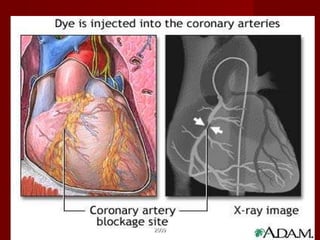
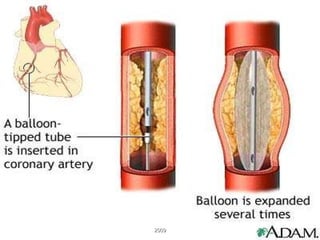
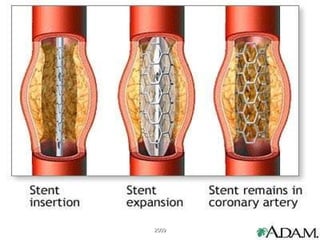
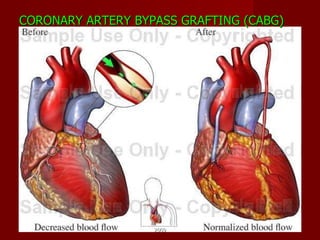
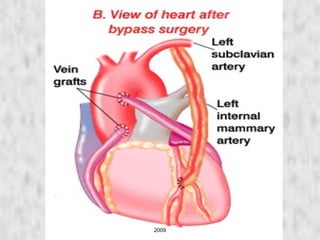
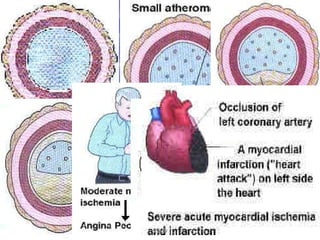
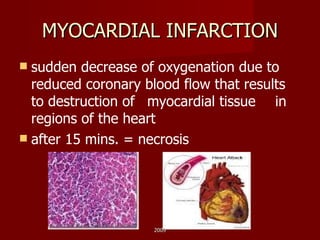
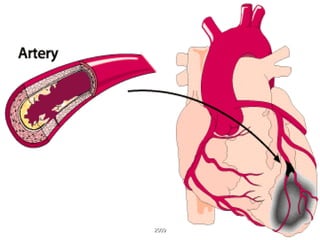
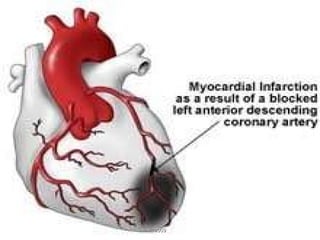
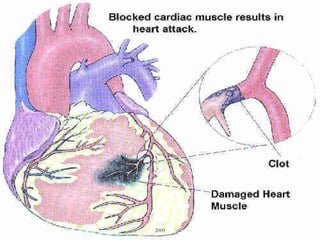
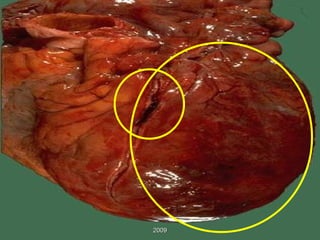
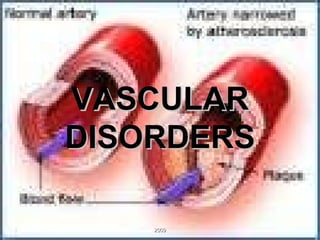
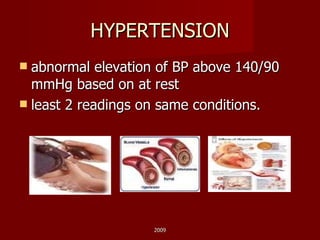
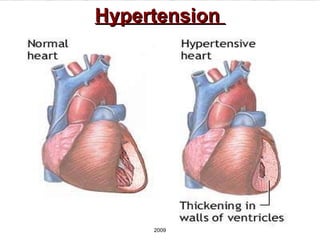
The document outlines a cardiovascular system course, covering anatomy and physiology of the heart and blood vessels, as well as history and assessment findings for cardiac diseases. Key topics include heart structure and function, blood supply, blood pressure control mechanisms, risk factors for heart disease, physical exam techniques, diagnostic tests, and common cardiac conditions such as coronary artery disease, heart failure, and infectious or inflammatory disorders of the heart.