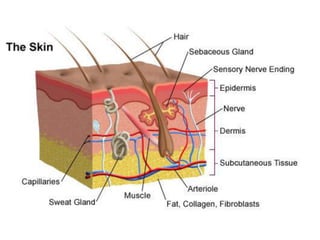
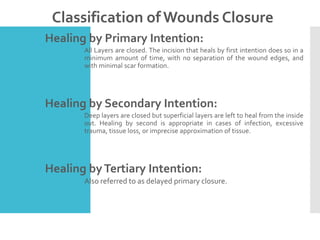
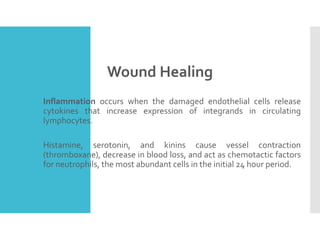
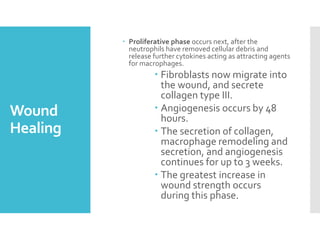
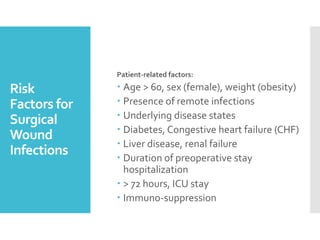
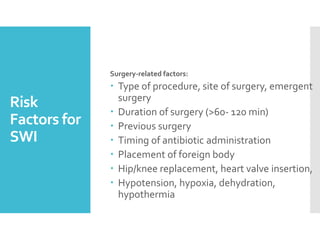
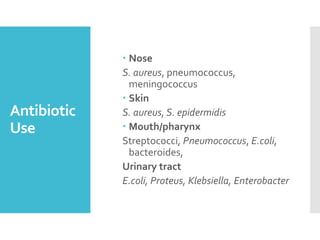
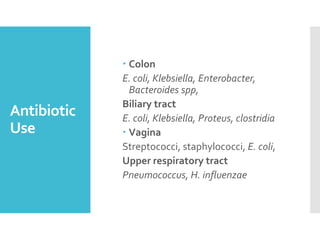
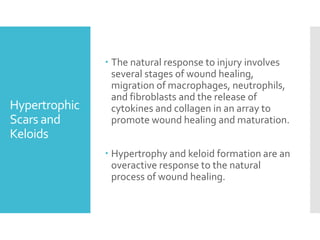
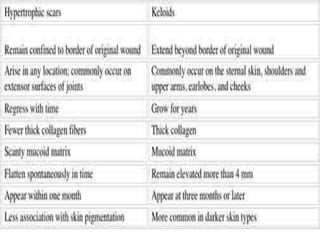
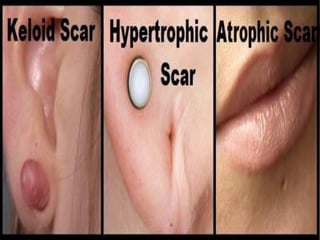
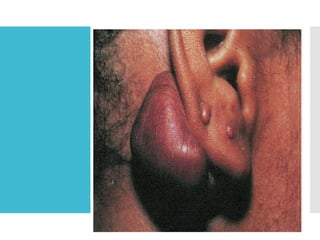
Wound healing is a complex process involving inflammation, proliferation, and maturation, classified into distinct phases and types of wounds. Factors influencing surgical wound infections include patient-related and surgery-related aspects, with specific bacteria associated with different body regions. Hypertrophic scars and keloids are abnormal wound healing responses, with distinct characteristics and treatment options such as pressure therapy and corticosteroid injections.