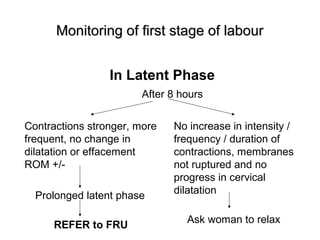
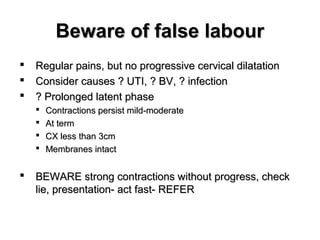
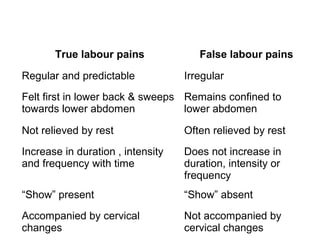
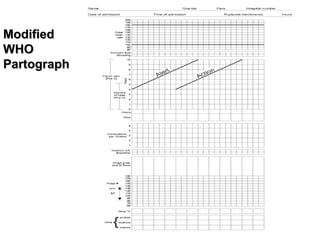
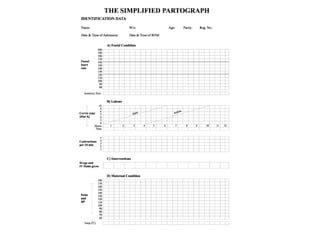
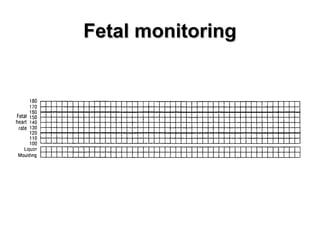
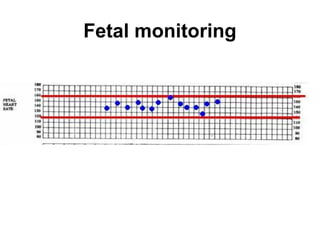
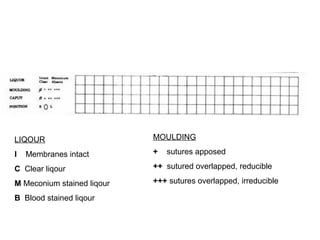
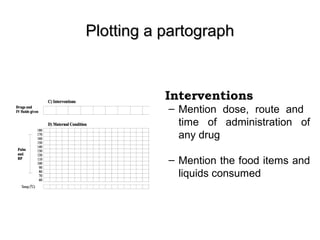
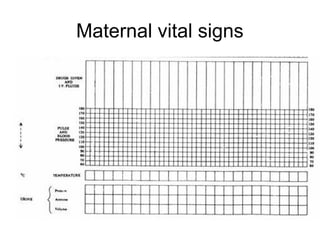
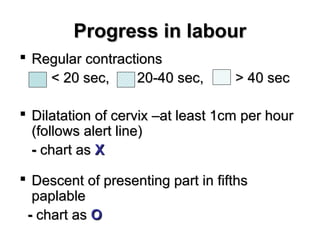
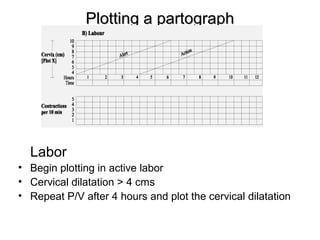
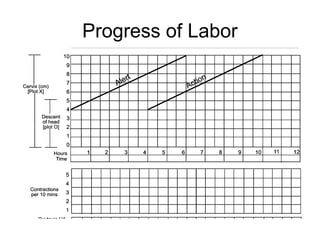
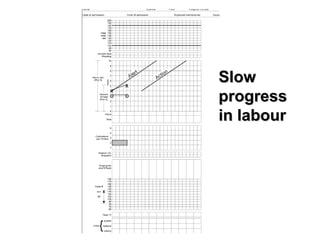
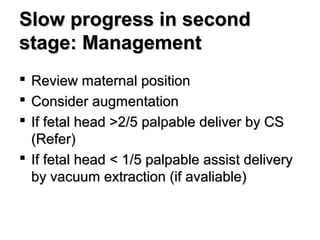
The document discusses how to use a partograph to monitor labor progress and recognize signs of slow labor. It explains that a partograph is a graphical record of labor that should be started once a woman is in active labor. The document outlines how to plot cervical dilation, descent of the baby, and other variables on the partograph. It emphasizes using alert and action lines to identify slow labor progression. If those lines are crossed, it recommends interventions like oxytocin augmentation or referral for cesarean delivery to prevent obstructed labor.