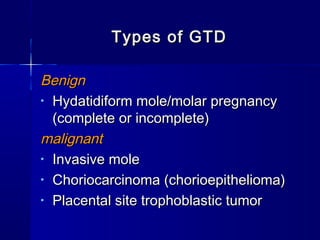
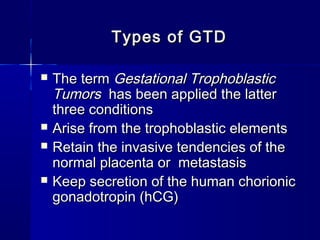
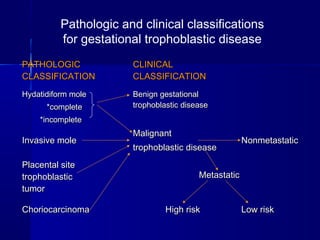
This document discusses gestational trophoblastic disease (GTD), including types like hydatidiform mole. It provides details on:
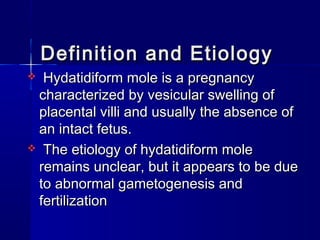
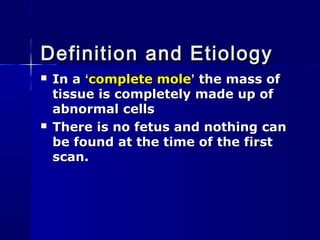
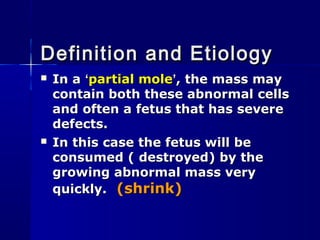
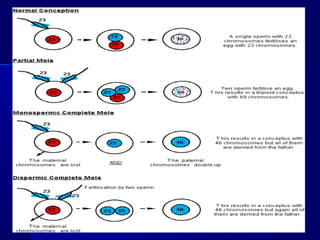
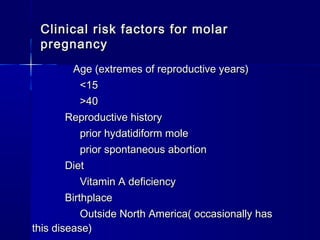
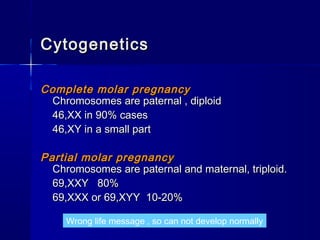
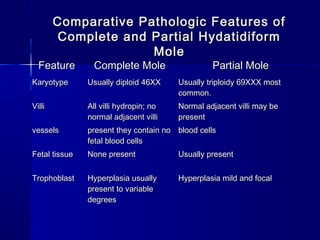
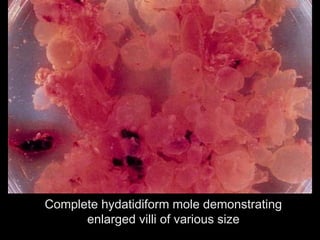
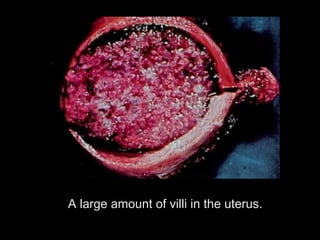
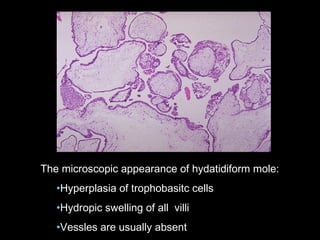
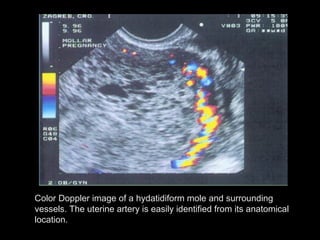
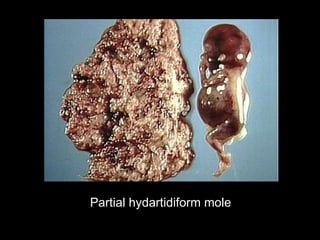
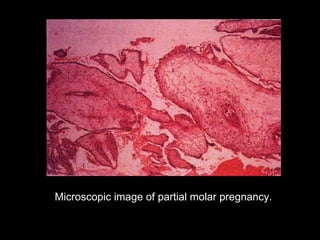
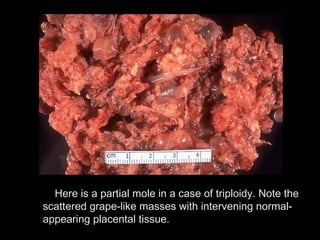
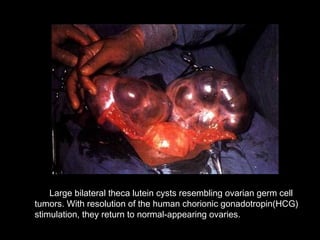
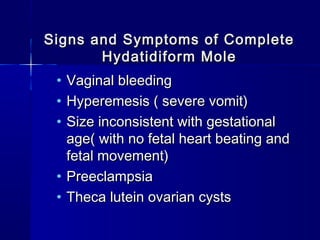
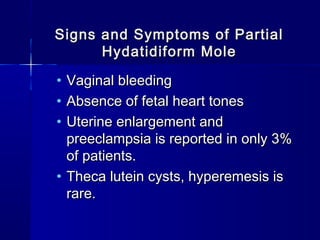
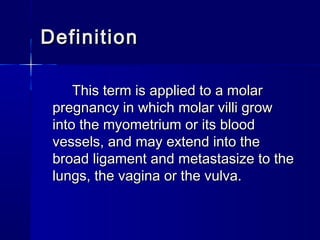
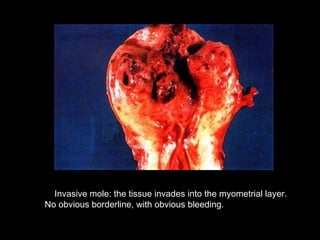
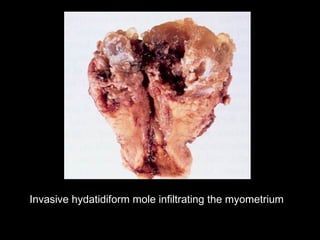
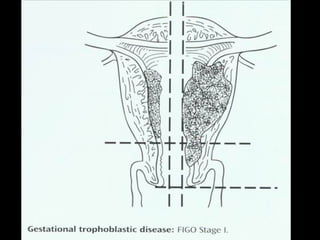
- Hydatidiform mole (molar pregnancy) which is characterized by vesicular swelling of placental villi and absence of an intact fetus. It can be complete or partial.
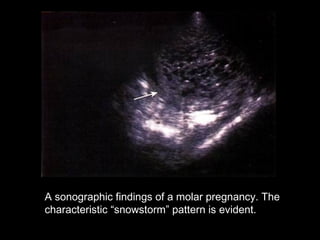
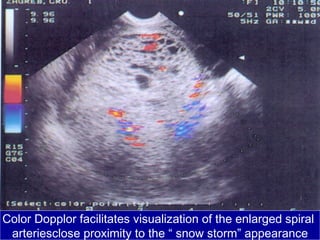
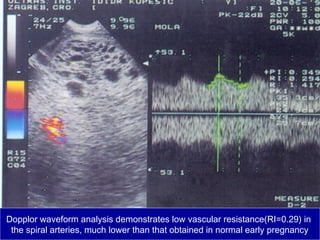
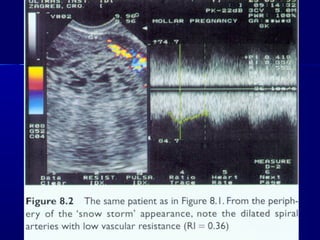
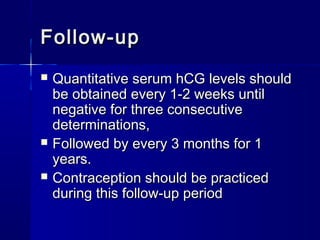
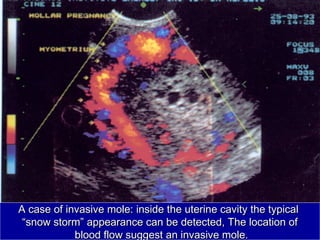
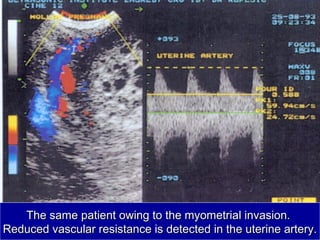
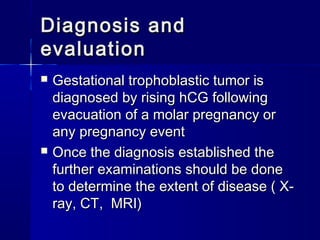
- Diagnosis involves quantitative beta-HCG testing and ultrasound showing a "snowstorm" pattern. Symptoms include vaginal bleeding.
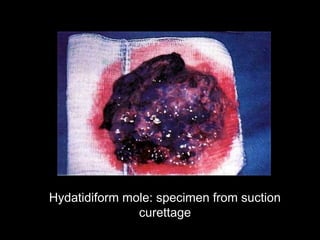
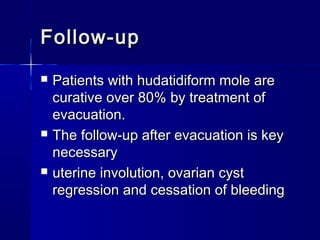
- Treatment is suction dilation and curettage to remove benign hydatidiform moles. Precautions like oxytocic agents after evacuation are recommended.