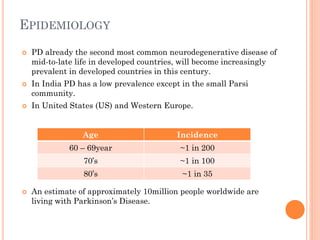
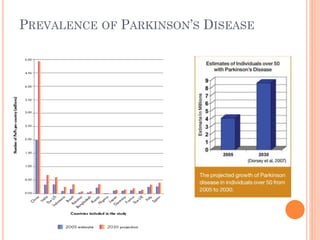
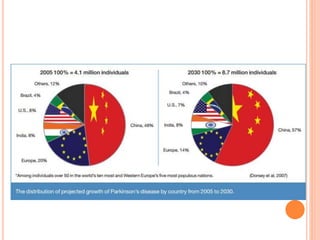
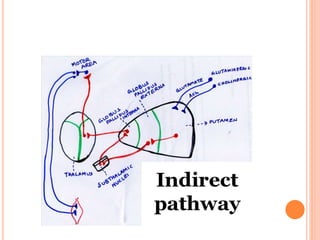
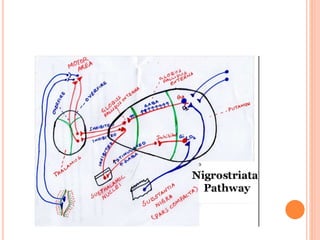
This document provides an overview of Parkinson's disease. It begins with definitions and discusses epidemiology, etiology, risk factors, types, signs and symptoms, pathophysiology, staging, complications, diagnosis, and pharmacotherapy. The key points are:
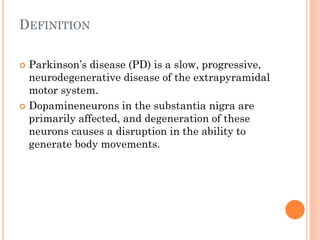
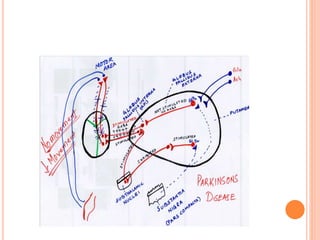
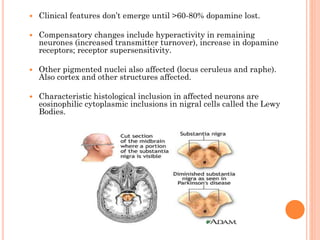
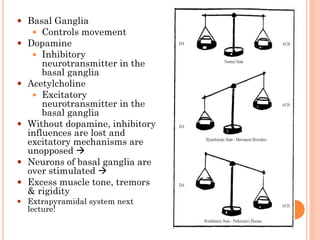
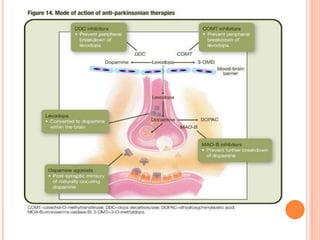
- Parkinson's disease is a progressive neurodegenerative disorder caused by loss of dopamine-producing neurons in the substantia nigra.
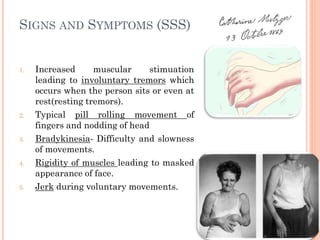
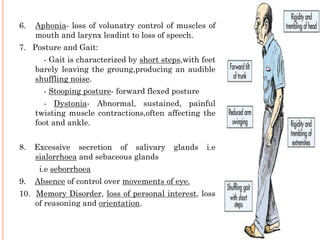
- Risk increases with age and family history. Symptoms include tremors, rigidity, bradykinesia, and postural instability.
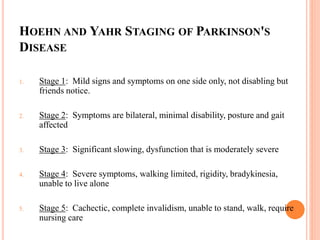
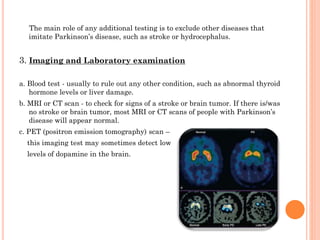
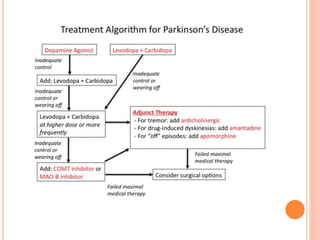
- Diagnosis is based on symptoms and response to levodopa treatment. Staging uses the Hoehn and Yahr scale.
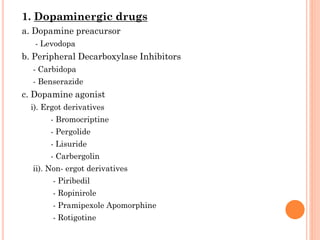
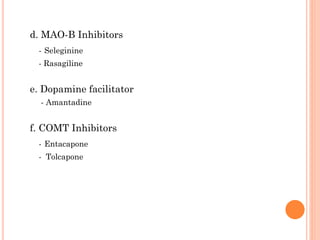
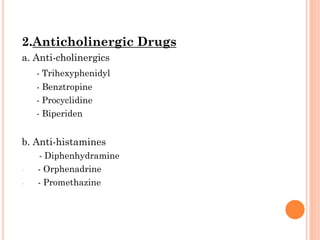
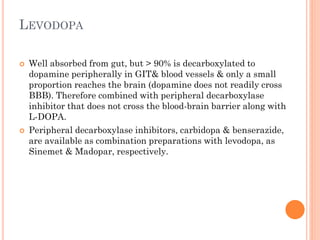
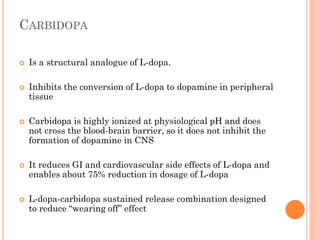
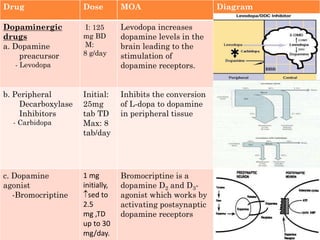
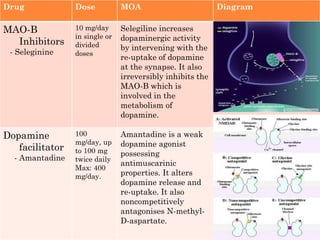
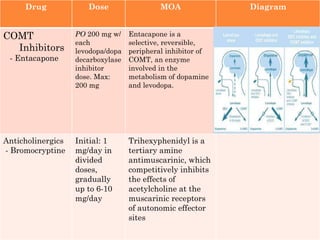
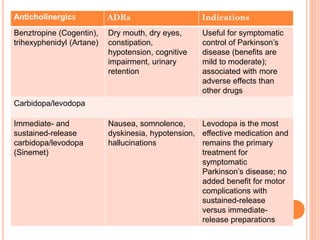
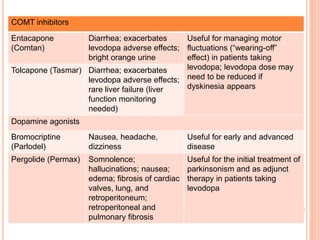
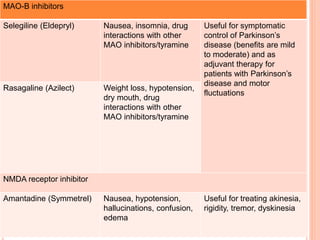
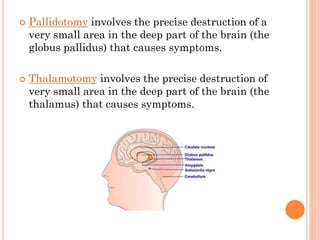
- Treatment focuses on dopamine replacement therapy